Unraveling Hope For Prion Disease And Other Progressive Neurodegenerative Diseases
(Posted on Thursday, June 9, 2022)
Prion diseases are rare but deadly neurodegenerative brain diseases that result from misfolding protein. Impacting both animals and humans, such rapidly progressive diseases result in abnormal physical and impaired mental functioning within months of diagnosis until death. Examples include mad cow disease, scrapie, Kuru, and Creutzfeldt-Jakob disease.
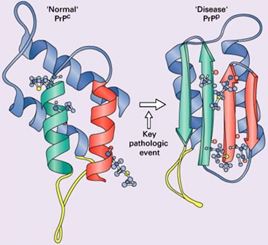
Figure 1: Conversion of a normal PrPc protein into the disease-causing prion PrPSc. FROM “PRION PROTEIN DISEASE AND NEUROPATHOLOGY OF PRION DISEASE” DU PLESSIS 2008.
The normal cellular host protein PrPC holds an intrinsic property to fold. When it folds differently, the protein undergoes a conversion to the pathogenic PrPSc conformation (Figure 1). Specifically, the protein loses some of its alpha helical nature and becomes greatly composed of beta-pleated structures, which are prone to aggregation. The infectious particle can consequently accumulate in the brain and have detrimental impacts in cognition. PrPSc also replicates like an inanimate crystal; devoid of genetic material, PrPSc auto-catalyzes and triggers a chain-like reaction to produce more of itself. PrPSc is also known to ravage through the brain, creating a sponge-like (spongiform) appearance.
At present, there are no cures available to treat prion disease. Novel work done by Mead et al. however provides a glimmer of hope regarding an approach to treat patients with Creutzfeldt-Jakob disease.
They designed a monoclonal antibody as a potential treatment for Creutzfeldt-Jakob disease. However, unlike most others who create antibodies that bind to aberrant protein, Mead and colleagues designed an antibody that stabilizes the normal protein precursor. If successful, this may prove to be a valuable approach for treatment for a number of similar diseases, including Alzheimer’s.
What is Creutzfeldt-Jakob disease?
Creutzfeldt-Jakob disease is a rapidly progressive neurodegenerative disease that causes dementia and ultimately death. This devastating disease affects one person per million per year. In the United States, that is roughly 320 cases annually. However, because it is very difficult to diagnose, researchers and health care professionals speculate that its prevalence may be inaccurate.
There are four types of Creutzfeldt-Jakob disease: sporadic Creutzfeldt-Jakob disease, genetic Creutzfeldt-Jakob disease, variant Creutzfeldt-Jakob disease, and iatrogenic Creutzfeldt-Jakob disease. Sporadic Creutzfeldt-Jakob disease is the most common form of Creutzfeldt-Jakob disease, accounting for 85% of cases, but its causes are unknown. Whereas genetic Creutzfeldt-Jakob disease results from an inherited mutation from one or both parents. This form represents 10% to 15% of patients. Variant Creutzfeldt-Jakob disease comes from exposure to bovine spongiform encephalopathy (BSE), most often through consumption of infected cattle. Iatrogenic Creutzfeldt-Jakob disease is reported to be the least common type of Creutzfeldt-Jakob disease, representing less than 1% of cases. Patients contract the disease through exposure to contaminated medical equipment or medical procedures.
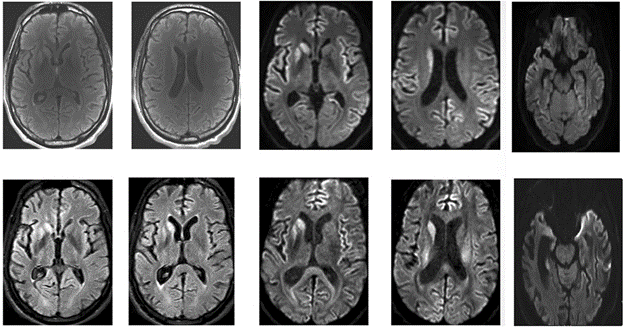
Figure 2: A FLAIR and Diffusion MRI scans of the horizontal sections of the brain of a 33- year old patient with sporadic Creutzfeldt-Jakob disease (Creutzfeldt-Jakob disease). Top row are MRI scans of the patient’s brain taken in April 2016. Bottom row are MRI scans of the patient’s brain taken in May 2016. WIETSE ET AL. 2018.
In their study that spanned from mid-October 2018 to July 2019, Mead and colleagues investigated the effect of PRN100, an antibody to PrPC, on Creutzfeldt-Jakob disease progression. The study consisted of six patients: five patients were clinically diagnosed with probable sporadic Creutzfeldt-Jakob and one patient was clinically diagnosed with iatrogenic Creutzfeldt-Jakob disease.
Patients followed a gradual dosing schedule of PRN100 and were assessed using the MRC Disease Rating Scales. Beginning at 1 mg/kg, PRN100 doses were administered in 2 to 6 day increments with the maximum dosage of 80 to 120 mg/kg administered every two weeks. Their scores were then compared to those obtained from the National Prion Monitoring Cohort observational study that served as controls. Based on literature precedent, researchers aimed for a 50nM concentration of PRN100 in the cerebrospinal fluid.
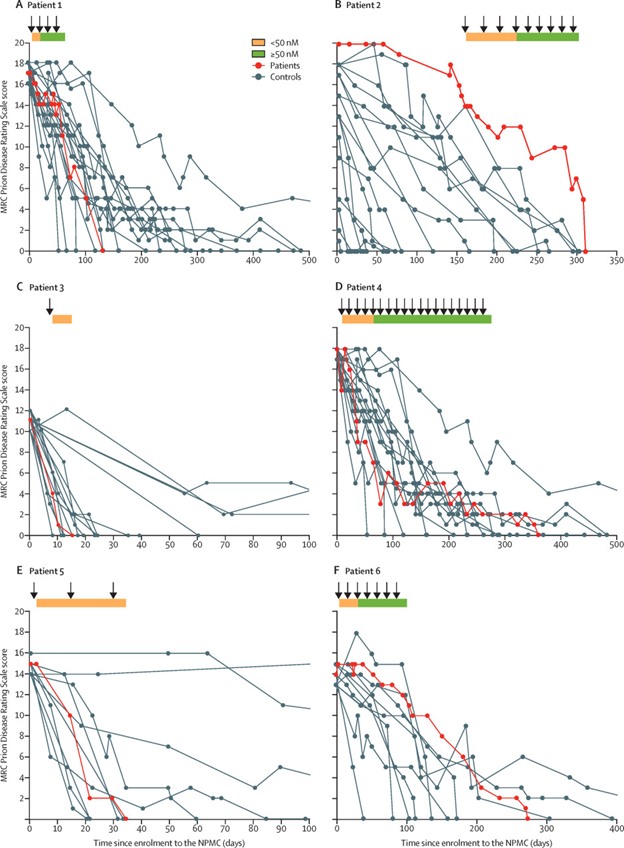
Figure 3: Patients’ MRC Prion Rating Scale scores over time (days) since enrollment. Panel (A) represents scores of patient 1(red) compared to 18 controls (gray) with sporadic Creutzfeldt-Jakob with a heterozygous genotype codon on the PRNP gene and baseline score on the MRC Prion Disease Rating Scale within 16-18. Panel (B) represents scores of patient 2 (red) to 17 (gray) controls with iatrogenic Creutzfeldt-Jakob, any genotype codon on the PRNP gene and any score on the MRC Prion Disease Rating Scale. Panel (C) represents scores of patient 3 (red) compared to 17 controls (gray) with sporadic Creutzfeldt-Jakob, a baseline score of 10-12 on the MRC Prion Disease Rating Scale and a genotype at codon 129 in the PRNP gene. Panel (D) represents scores of patient 4 (red) compared to 18 controls (gray) with sporadic Creutzfeldt-Jakob with a score of 16-18 on the MRC Prion Disease Rating Scale and a heterozygous genotype at codon 129 on the PRNP gene. Panel (E) represents scores of patient 5 (red) compared to 10 controls (gray) with sporadic Creutzfeldt-Jakob, a baseline score of 12-15 on the MRC Prion Disease Rating Scale, and a methionine homozygous genotype at codon 129 in the PRNP gene. Panel (F) represents scores of patient 6 (red) to 10 controls (gray) with sporadic Creutzfeldt-Jakob, a baseline score of 13-15 on the MRC Prion Disease Rating Scale, and a heterozygous PRNP genotype at codon 129 in the PRNP gene. The orange bar represents a concentration lower than 50nM of the PRN100 antibody in the cerebrospinal fluid. The orange bar represents a concentration equal to or greater than 50nM of the PRN100 antibody in the cerebrospinal fluid.
Mead et al 2022
With a small sample size and limited stock of drug availability in mind, researchers saw promise in the preliminary data. Two patients passed away before 50nM of PRN100 was reached (patients 3 and 5, both of whom were diagnosed with sporadic Creutzfeldt-Jakob disease); however, the scores from the MRC Prion Disease Scales from three patients did stabilize when there was a 50nM or higher concentration of PRN100 (figure 3). Their careful gradual dosing approach contributed to the average of 47 days to reach 50nM of PRN100 in the cerebrospinal fluid and clinically significant neurological decline among patients with sporadic Creutzfeldt-Jakob disease during that period. For additional context, the median survival for patients with sporadic Creutzfeldt-Jakob disease in the National Prion Monitoring Cohort observational study was 25 days from their respective enrollment into the study.
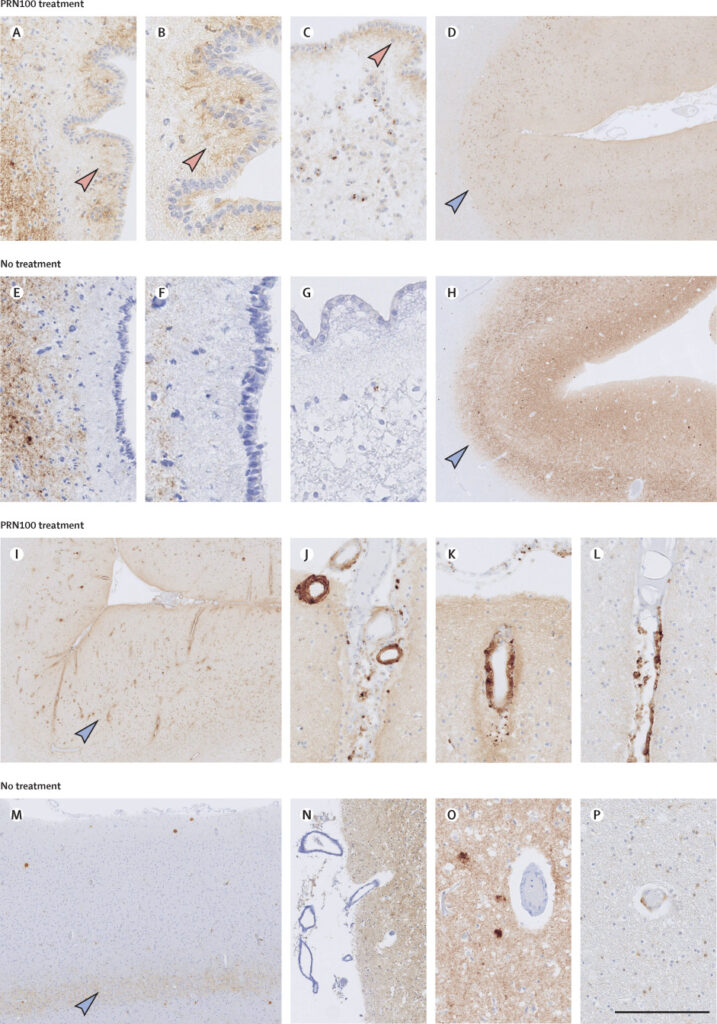
Figure 4: The impact of PRN100 on the removal of PrPSc from the brain. Panels A-D come from PrP labeling in the brain of PRN100 treated patient 2. Panels E-H are PrP labeling of the brain of an untreated patient with iatrogenic Creutzfeldt-Jakob. Panels I-L compare the optical region of the PRN100-treated brain of patient 2. Panels M-P compare the optical region of the non-treated brain of a patient with iatrogenic Creutzfeldt-Jakob. Mead et al 2022
Based on the autopsy of patients 2 and 3 (diagnosed with iatrogenic and sporadic Creutzfeldt-Jakob disease, respectively) reported no evidence of cytotoxicity, lymphocytic inflammation, or increased formation of vacuoles. There was a striking decrease in PrPSc immunoreactivity in the parietal and occipital cortex, change in PRPSc distribution in the subventricular areas, and an accumulation of amyloid in the arteries in the brain (cerebral amyloid angiopathy) in patient 2 compared to the untreated patients with iatrogenic Creutzfeldt-Jakob disease (figure 4). Mead and colleagues attributed the cerebral beta amyloid angiopathy to be the result of treatment, however, they report no amyloid-related imaging abnormalities in any patient. The autopsy of patient 3 also had different PrP labeling in the periventricular regions in comparison to the historical controls. Mead and researchers also observed PRN100 in the patient’s brain tissue to be similar in concentration observed in the cerebrospinal fluid (well above concentrations shown to clear cells of PRPSc infection).
Although their results are highly preliminary, it does seem that the alternative approach of Mead et al stabilizing the normal protein that is the pathogenic form may be promising for a large number of neurological diseases.
Read original article on Forbes here.

