A Ray Of Hope For Treatment Of Covid-19
(Posted on Friday, November 13, 2020)
New reports on the effectiveness of two different monoclonal antibody therapies have given us a ray of hope that we can prevent Covid-19 from turning deadly. In these preliminary reports both antibody drugs seem to reduce hospitalization for patients if the drugs are given early in the course of the disease. Other studies have shown that administering these same drugs after the disease progresses does little to no good. This finding points us towards two important steps we need to take to effectively contain the pandemic by as soon as next summer.
The two therapies—one from Eli Lilly and the other from Regeneron—work directly on the virus to prevent it from replicating. For Covid-19, the virus acts in three distinct phases. The first phase takes place a few days to a week following infection. During this period, virus growth is slow. In the second phase, virus growth is rapid and the concentration of virus particles in nasal fluids, the lung, and the intestine is high. This is normally when patients begin to show symptoms, after the peak of virus replication. At this point, we enter the third phase. It is this phase that life-threatening symptoms unroll over a matter of two to three weeks and sometimes longer. Little to no infectious virus is present but the disease the virus started continues on.
As might be expected, antiviral drugs such as the monoclonal antibodies seem to work only in the initial two phases, usually before a patient is hospitalized. This means that for the drugs to be administered early enough to be effective, those exposed to the virus must be tested regularly, whether or not they show symptoms of disease or not. An early positive result can lead to early treatment that might save a life. This is hopeful and promising news and is encouraging for the array of new chemically based antiviral drugs currently in early stages of clinical development.
But the treatment isn’t without drawbacks. First, the treatment needs to be administered by infusion—it’s not a quick injection that can be over and done in a few minutes at your regular walk-in clinic. Second, monoclonal antibodies are very expensive to manufacture. They are among the most expensive drugs on the market today. President Trump reportedly received an eight gram treatment of Regeneron—about two heaping teaspoons. The cost for that treatment—if we assume costs similar to those of other monoclonal antibody treatments like Keytruda, which is used for certain types of cancer—would be over four hundred thousand dollars.
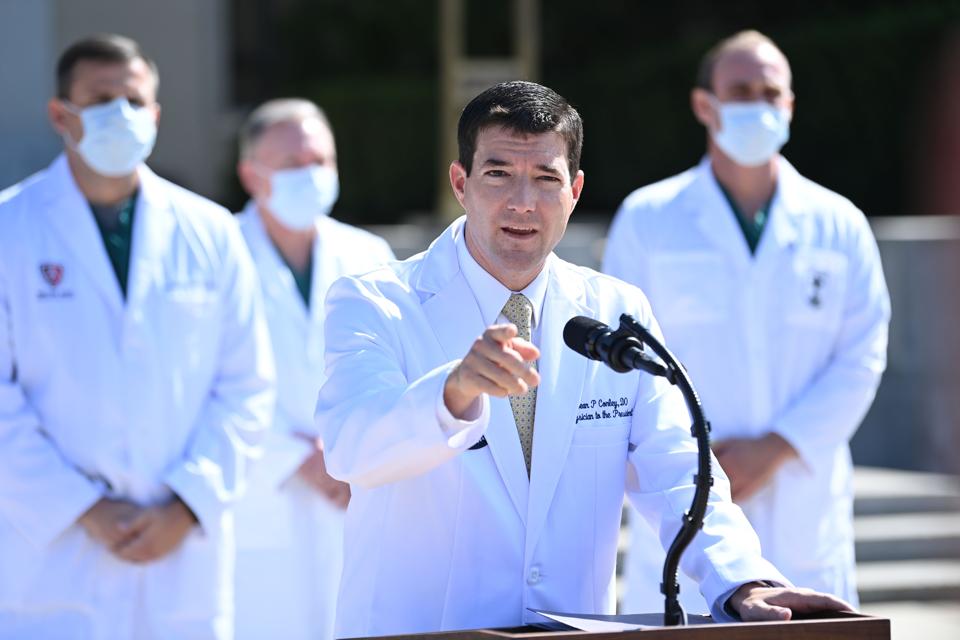
TOPSHOT – White House physician Sean Conley answers questions surrounded by other doctors, during an update on the condition of US President Donald Trump, on October 4, 2020, at Walter Reed Medical Center in Bethesda, Maryland. – US President Donald
AFP VIA GETTY IMAGES
There was also a worrying finding from the Lilly trail. Even over the short course of treatment some patients developed resistant variants. As with many viruses such as HIV, combinations of antiviral drugs each directed to a different target may do the job.
These drawbacks, combined, make monoclonal antibody treatments impractical for treating the large numbers of people in the United States infected today. Even if the cost of the drugs themselves wasn’t a challenge, manufacturing issues would be. There are only about 50,000 doses of Regeneron available in the US today, which would cover just over half of the number of newly infected Americans yesterday.
Still, there is hope. The Eli Lilly and Regeneron treatments have demonstrated proof of principle. Drugs that prevent replication of SARS-CoV-2 can prevent early SARS-CoV-2 from progression to serious disease if administered early on in the course of the disease. Now, we must do two things urgently.
First, we must focus on developing chemically based antivirals that use a similar approach but are cheaper and easier to manufacture. These drugs exist and early prototypes have already been proven effective in lab settings against MERS, SARS, and SARS-CoV-2. Now we must accelerate efforts to safely move these treatments out of the labs and into clinical trial settings.
Second, and perhaps more importantly, we must ensure we have a system in place to identify those newly infected as early as possible. This can only be done if we make rapid, five-minute antigen tests universally available, so every person potentially exposed can quickly assess whether they are infected or not.
The only way to ensure these two critical steps are taken is through the power of the federal government. Through the course of this pandemic, the Trump administration has chosen not to use the full weight of our national powers to propel the containment effort, instead leaving it to states to pull together a piecemeal approach. This should not stand. A massive, nationally coordinated testing strategy should be implemented immediately while federal resources are pulled together to help fast-track cheaper monoclonal antibody treatments.
If we did these two things, we could end this pandemic by next summer. If not, let us prepare ourselves for Covid to control us not just next year but potentially for a few more years to come.
This article originally appeared on Forbes.
Originally published on November 13, 2020.

