Why Patterns In Covid-19 Variation Might Resemble Seasonal Flu
(Posted on Thursday, January 21, 2021)
Random variation is an essential component of all living things. It drives diversity, and it is why there are so many different species. Viruses are no exception. Most viruses are experts at changing genomes to adapt to their environment. We now have evidence that the virus that causes Covid, SARS-CoV-2, not only changes, but changes in ways that are significant. This is the eighth part of a series of articles on how the virus changes and what that means for humanity. Read the rest: part one, part two, part three, part four, part five, part six, and part seven.
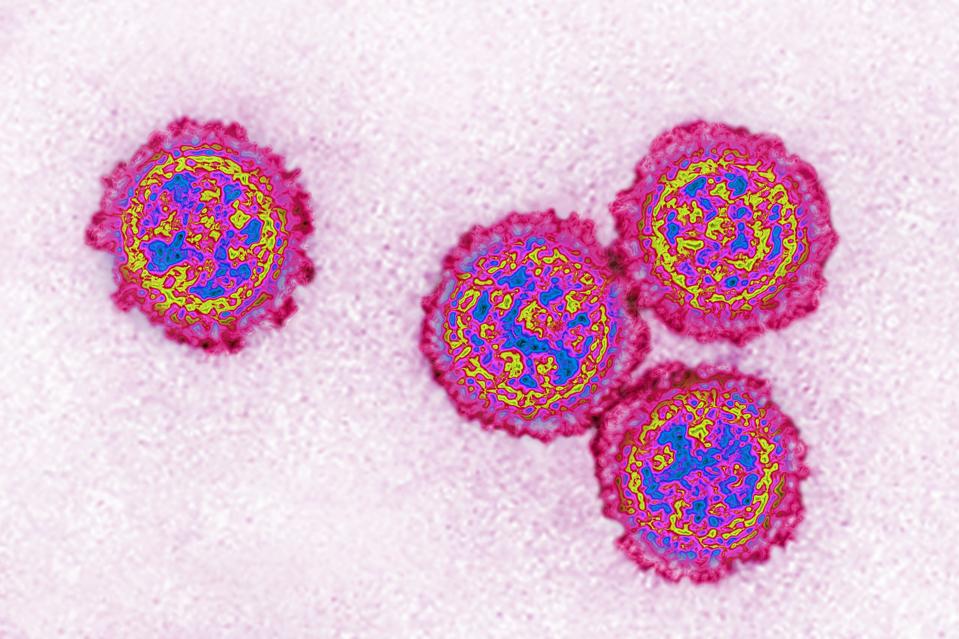
Influenza virus (from the Orthomyxoviridae family and the Influenzavirus genus). Image made from a transmission electron microscopy view. (Photo by: Cavallini James/BSIP/Universal Images Group via Getty Images)
UNIVERSAL IMAGES GROUP VIA GETTY IMAGES
We’ve learned that some variants of SARS-CoV-2 are more transmissible. Equally troubling is the possibility that future variants — or ones currently circulating off our radar — will in some way compromise our natural immune response, complicating our ability to treat critically ill Covid-19 patients with the antibodies of those who recovered from the disease. In my previous story for this series, I discussed how the evolution of human coronaviruses more broadly gives us insight into what we might expect from SARS-CoV-2. The same is true of influenza viruses.
Waves of influenza, like cold-causing coronaviruses, don’t come and go at random. They’re seasonal, recurring in patterns we can anticipate and plan interventions around after tracking them for many years. This we know. Why, though, do the dominant strains of influenza vary from one year to the next? Is there a linear evolutionary pathway to be traced from one strain to another, just as we’re attempting to do with SARS-CoV-2?
A study published in 2017, coauthored by some of the same researchers behind the preprint on coronavirus evolution I analyzed previously, proposes a theory of influenza evolution that might just apply to Covid-19, too. According to this theory, the viruses that cause both diseases evolve across multiple scales — in individuals, between individuals, and around the globe.

Seasonal variation of human coronaviruses in Stockholm, Sweden. Test results between 2010 and 2019.
POTENTIAL IMPACT OF SEASONAL FORCING ON A SARS-COV-2 PANDEMIC DOI: HTTPS://DOI.ORG/10.4414/SMW.2020.20224 PUBLICATION DATE: 16.03.2020
Surveillance of seasonal influenza viruses from 2004 to 2008.
CDC 2007-08 U.S. INFLUENZA SEASON SUMMARY HTTPS://WWW.CDC.GOV/FLU/WEEKLY/WEEKLYARCHIVES2007-2008/07-08SUMMARY.HTMMost of us, when we catch either of these viruses, will develop a transient infection — meaning the duration of our sickness has a definite beginning and end. But a small fraction of people develop prolonged infections, either stretching on for weeks or months without pause or subsiding only to return with a vengeance. Chinese health authorities estimate that for Covid-19, this population of long-term shedders is as high as five percent.
The reasons for persistence of infection vary, and in some cases elude us. One explanation consistent with both Covid-19 and the flu is that some patients are immunocompromised, unable to generate an immune response vigorous enough to clear out the virus once and for all. It is also the case that either virus, if allowed an extended stay in a human host, has more time and space to alter itself in advantageous ways. Single mutations, as well as multiple co-occurring mutations, can change the face of the viral genome and, once replicated enough, become the norm, rather than the exception. In other words, an immunocompromised host gives the virus, which mutates constantly anyway, an opportunity to incubate a better version of itself — and by that I mean better for the virus, not necessarily us.
We’ve already seen this process in action with SARS-CoV-2. Early on in this series, I described a case study of a man who was hospitalized twice with Covid-19, first in May then in August of 2020. Prior to contracting the virus, the man was already living with lymphoma and receiving treatment known to have immunosuppressive effects. He eventually succumbed to the disease, but before he did researchers sampled and sequenced the virus in his body more than 20 times. Remarkably, some of the mutations they observed in his viral RNA can now be found in the SARS-CoV-2 variants currently circulating around Europe, South America, and other parts of the world. One example is the H69-V70 deletion, a mutation of the N-terminal domain also seen in the so-called UK variant B.1.1.7.
The 2017 study documents the same phenomenon, but with the influenza virus. Using samples from not one but four immunocompromised cancer patients, all who had prolonged flu infections, the researchers observed the same mutations arising frequently and independently in multiple hosts. For SARS-CoV-2, mutations that occur in and around the spike protein — which the virus uses to bind to and hijack our cells — have been the primary focus and worry. In the influenza genome, it was another surface protein known as hemagglutinin that researchers flagged as a hotspot for variation. In both cases, specific mutations occur in specific places in viral genomes found in specific patients — in addition to being identified in variants that occur globally. The researchers studying the flu called these “parallel mutations.”
There are two possible explanations for why parallel mutations occur. One option is that new variants of SARS-CoV-2 and influenza actually have their origins in immunocompromised patients. The other — less linear, more diffuse — option is simply that a virus’s drive and tendency towards change is as active and dynamic in the human body as it is in human populations. Either way, it begins to make more sense that the same infinitesimal changes to SARS-CoV-2, in some cases limited to a single amino acid, are popping up in different parts of the world. Expose the virus to similar selective pressures and challenges — namely, partial immunity — and it will adapt in similar ways.
If I were to make a prediction based on what we’ve seen of SARS-CoV-2 and its capacity for variation so far, I’d say it is much more like influenza than any other virus we know of. To prepare ourselves accordingly, we must adjust our vaccine development pipelines and public health interventions more broadly to account for emergent and future variations. Otherwise we’ll be setting ourselves up to be blindsided yet again — against our best interests, and in favor of the virus’s.
Originally published on Forbes (January 21, 2021)

