A Tale Of Two Viruses
(Posted on Monday, January 25, 2021)

TOPSHOT – A morgue attendant at the Johannesburg branch of the South African funeral and burial services company Avbob keeps the curtain open from inside a refrigerated container where bodies of patients deceased with COVID-19 related illnesses are
AFP VIA GETTY IMAGES
As we enter the last week of January, much uncertainty remains around how new variants of the Covid-19 virus, SARS-CoV-2, will shape the year ahead of us. Reports from British officials that B.1.1.7, the so-called UK variant, isn’t just more transmissible than its predecessors but more lethal as well are raising equal parts alarm and skepticism, especially since the same variant has spread to at least 60 countries and is now dominant in a few. Meanwhile B.1.351—the so-called South Africa variant, formerly known as 501.V2—has become so widespread as to prompt the Biden administration to consider imposing a travel ban on non-US citizens hailing from South Africa.
Researchers around the world are not just hustling to sequence these new variants (as of last week, in the US only 0.3 percent have been identified), but conduct studies and experiments that can help answer lingering questions about their impact on natural immunity, vaccines, and the duration of the current pandemic. Two recent publications, both still undergoing peer review, add some depth and nuance to our current understanding of B.1.1.7 and B.1.351—demonstrating that viral variation isn’t an inherently disastrous development, but could become one if we don’t adequately anticipate and address its consequences.
The variant B.1.1.7: A match for vaccines?
The first of the two studies, conducted by Pfizer and BioNTech employees in Germany and the US, investigated whether the B.1.1.7 variant could still be countered by vaccines, specifically the Pfizer-BioNTech vaccine used predominantly in the UK. The conclusion? The variant is likely to be neutralized, but further research and data is needed to be sure.
The B.1.1.7 variant was first identified in September 2020 but only really entered the spotlight months later, when its prevalence in the UK and elsewhere rapidly increased. Genome sequencing indicates that B.1.1.7 has eight mutations that change the shape of its spike (S), the protein that helps it bind to host cells. These mutations, specifically the N501Y mutation, allow the virus to bind even more tightly than usual, fueling worries that a vaccine built around the genomic architecture of the spike would lose its potency.
In an attempt to quell these concerns, the researchers behind the study introduced different mutations exhibited by B.1.1.7 to pseudoviruses created in the laboratory that contained the SARS-CoV-2 spike. They also drew antibodies from the blood of 16 people inoculated with the Pfizer-BioNTech vaccine. Fortunately, they found that these antibodies, administered in concentrations similar to those that neutralize older variants, could still deactivate the lab-mutated virus—excellent news that should calm the nerves of many preparing to receive the vaccine.
It must be emphasized, however, that how non-replicating pseudoviruses react to antibodies in a controlled experiment might differ from how SARS-CoV-2 behaves in the real world. That’s why, in their concluding remarks, the researchers emphasize the need for further research.
The variant B.1.351: Immune resistant?
The second of the two studies focuses on B.1.351, rather than B.1.1.7. Conducted by a group of researchers working in South Africa, the country where the variant was first detected, the study tests whether immunity developed against previous strains of SARS-CoV-2 would remain sufficiently protective against B.1.351. The results suggest, regrettably, that this might not be the case.
In addition to increasing the binding abilities of the virus like N501Y, some mutations like K417N and E484K might have the added ability to cause or promote immune resistance or escape. Mutations associated with the E484 site in particular have, at least in one study, reduced the protective capabilities of some antibodies more than tenfold.
To assess whether this was true of the B.1.351 variant as a whole, the South Africa-based researchers gathered viral samples from Covid-19 patients who were infected by the Wuhan strain during the summer, as well as from patients infected by the B.1.351 variant mid-November, and grew them in the laboratory. Then they gathered plasma samples that contained neutralizing antibodies from patients who were infected by, then recovered from, the older strain.
As might be expected, the virus from the first wave was slowly and steadily neutralized as the dilution of plasma increased. But pitted against samples of the B.1.351 variant, the plasma didn’t appear to have the same neutralizing effect. As the concentration of antibodies increased, the virus remained intact. This lack of efficacy is painfully apparent in the charts and images of petri dishes below.
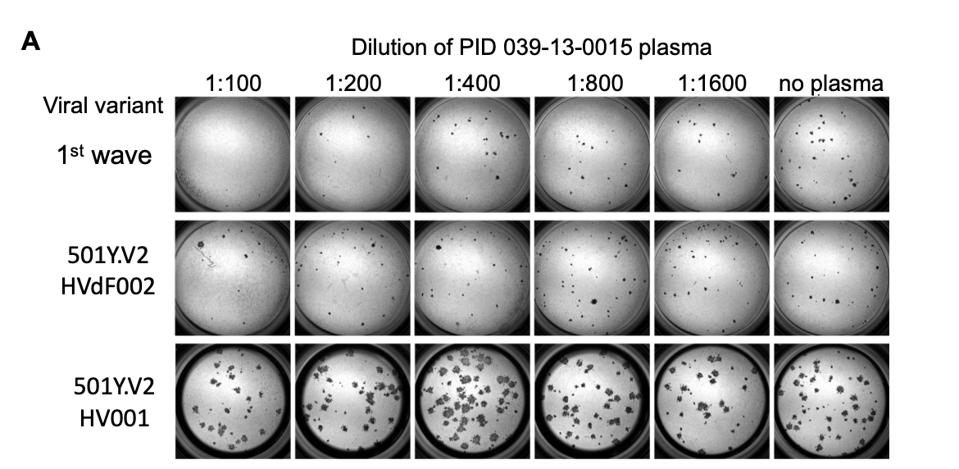
A representative focus forming assay using plasma from participant 039-13-0015.
ESCAPE OF SARS-COV-2 501Y.V2 VARIANTS FROM NEUTRALIZATION BY CONVALESCENT PLASMA HTTPS://WWW.KRISP.ORG.ZA/MANUSCRIPTS/MEDRXIV-2021-250224V1-SIGAL.PDFBased on their observations, the researchers concluded that new strains mount significant resistance against older neutralizing antibodies. Their closing remarks raise caution that just because you’ve been infected with SARS-CoV-2 before does not mean you are immune to reinfection, specifically with this new strain. Additionally, the currently distributed vaccines that target the S-protein of previous strains may not carry protection over to B.1.351.
Viral variation: Piecing together the bigger picture
At first glance, it might appear these studies are at odds, examining two distinct variants with two distinct methods. The first also directly involves a vaccine, while the second doesn’t. But both get at the same fundamental question—whether new variants of SARS-CoV-2 are adapting more rapidly to us than we are to them. They also have the same fundamental limitation, which is being confined to the laboratory. The first uses a pseudotype virus; the second, lab-cultured tissue. Excellent substitutes, in other words, but not the real thing.
Until we have long-term clinical data on vaccine efficacy and reinfection—another indicator of the effectiveness of natural immunity—we won’t be able to answer this question with certainty. That the Pfizer-BioNTech vaccine appears to counter the mutations that constitute the B.1.1.7 variant is certainly a good sign. Moderna, the company behind the only other Covid-19 vaccine currently approved for use in the US, has also announced plans to accelerate development of a booster shot in light of a study they conducted that saw no change in their vaccine’s efficacy against B.1.1.7, but a five to tenfold reduction in its efficacy against B.1.351 pseudotyped viruses—results that must also be corroborated with infectious variant virions. This adds yet more complexity to the task of providing vaccine protection to people everywhere.
Given the mixed results, what we can do is be safe, rather than sorry, and move full speed ahead with current efforts to stop and prevent disease in the general population. So long as the virus continues to spread, it will continue to mutate, becoming potentially more infectious and immune resistant. The most effective way to try to defeat these variants, whether new or old, are measures we’ve been championing since nearly the beginning: wearing masks, social distancing, restricting large gatherings, and isolating the infected. Ramping up enforcement of these measures, as well as worldwide vaccine distribution, is the only way we might still get Covid-19 under control.
Originally published on Forbes (January 25, 2021)

