What Can We Learn From Australia’s Covid-19 Response?
(Posted on Friday, March 26, 2021)

MELBOURNE, AUSTRALIA – Melburnians adjust to normal life post COVID-19 lockdown. People enjoy outdoor dining along the Yarra River on November 19, 2020 in Melbourne, Australia.
GETTY IMAGES
Australia’s Covid-19 response has been the envy of many countries with Dr. Fauci recently praising the country for being a world leader on “containment and management of emerging variants”. Aside from a few brief snap lockdowns in certain states, most Australians have been enjoying a relatively normal life with the Broadway production of Hamilton recently opening in Sydney to full capacity theaters.
As of March 23, 2020, Australia has just five new cases of Covid-19. The majority of these new cases are not from community transmission but from the hotel quarantine system that houses Australian citizens returning from overseas. Even after experiencing a second surge of cases last year, Australia swiftly learned from its mistakes and cases never rose over 1,000 for a population of 25.36 million. All of this has been achieved without vaccinations. Australia only began its vaccination program on Feb 21, 2021, yet as you can see in the chart below (Figure 1) cases have remained low for almost six months. While Australia does have considerable advantages in terms of geographic isolation and population density there is still much we can learn from their response. Australia’s success proves that a strong public health response enforced by a democratic government focused on vigilant testing, tracing and quarantine is the key to fighting a pandemic.
As of March 23, 2020, Australia has just five new cases of Covid-19. The majority of these new cases are not from community transmission but from the hotel quarantine system that houses Australian citizens returning from overseas. Even after experiencing a second surge of cases last year, Australia swiftly learned from its mistakes and cases never rose over 1,000 for a population of 25.36 million. All of this has been achieved without vaccinations. Australia only began its vaccination program on Feb 21, 2021, yet as you can see in the chart below (Figure 1) cases have remained low for almost six months. While Australia does have considerable advantages in terms of geographic isolation and population density there is still much we can learn from their response. Australia’s success proves that a strong public health response enforced by a democratic government focused on vigilant testing, tracing and quarantine is the key to fighting a pandemic. Below I’ve outlined some of the key lessons from Australia’s response that can be applied globally.
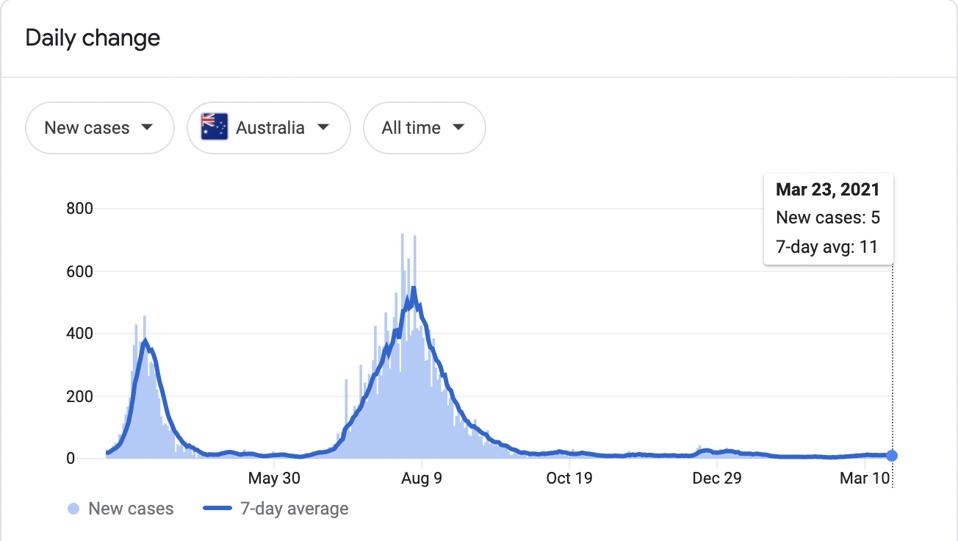
Figure 1: Covid-19 cases in Australia throughout the pandemic
JOHN HOPKINS UNIVERSITY VIA GOOGLE
1) Act quickly and decisively based on incoming data
When Covid-19 first became a real threat to Australia in March last year, the Federal government responded quickly closing international borders and implementing a mandatory home isolation program for returning Australian citizens. Police were dispatched to homes to check that returned travelers were adhering to quarantine requirements and when breaches were discovered, Australia quickly moved to a mandatory hotel quarantine system in which hotel rooms were often guarded by police or military. The states and territories also temporarily shut their borders down for the first time since 1919 during the Spanish flu pandemic.
These early border closures stopped the rapid spread of the virus and allowed for Australia to build a testing and tracing system that was not immediately overwhelmed and therefore very effective at controlling the spread of the virus. Closing state borders also meant that states like New South Wales and Western Australia were able to reopen their local economies after just two months of lockdown. The progress of individual states did not affect the entire country. State and territory borders have now reopened but international borders have remained closed due to the threat of the variants. Australia has also implemented a cap on incoming international flights carrying returned citizens in order to ensure the quarantine system isn’t overwhelmed. While this has been an effective policy it has not been without controversy. Approximately 40,000 Australians are currently stranded overseas, desperate for a place on those limited flights which has been considered a human rights violation by some.
Australia’s lockdown restrictions and behavioral safety protocols were also enacted swiftly. While restrictions varied between the states and rural and urban populations, they were clearly communicated through daily televised press conferences, public signage and advertising and further media outreach. Non-essential businesses were immediately closed, everyone was given a limited radius that they could not leave unless it was for essential work, medical appointments or caretaking, and households were not allowed to mix with some exceptions. Anyone found to be violating those restrictions faced a hefty fine. The easing of these restrictions and eventually restrictions on indoor and outdoor gatherings were tied to declining infection rates. This gave Australians a clear, logical path forward to reopening and encouraged compliance.
These swift, decisive actions have allowed Australia to reach zero cases at certain stages of the pandemic. When there is a small rise in cases (usually from workers at quarantine hotels) they have the systems in place to trace exposures and lockdown certain regions for a few days. With case numbers so low, the media is able to publish the exposure locations that the infected person visited in addition to traditional contact tracing. While there are a few complaints, the public is happy to comply with these brief lockdowns as they know that they will shortly return to the luxury of normal life.
2) Bipartisan unity is essential to an emergency response
Australia’s two major political parties are definitely still closer to the center than Republicans and Democrats but have grown increasingly combative in the last 10 years, with legislation often gridlocked in the two Houses of Parliament. However, when Covid-19 struck, they put aside their differences to work on a unified pandemic response. While Australia’s current conservative government normally clashes with the trade union movement, they recognized that union cooperation would be essential in implementing their emergency measures and gave them a role in shaping policy.
Early in the pandemic, the federal government introduced a $130 billion dollar economic bailout which included a six-month wage subsidy scheme. The legislation was rushed through Parliament in just one sitting day in order to get relief to Australians who needed it most. State leaders met in March 2020 to coordinate their responses and form a National Cabinet which would share data and strategies. Conservative Prime Minister Scott Morrison also preached a message of unity, saying “There are no blue or red teams. There are no unions or bosses. There are just Australians now”. The political truce between the parties did not outlast the crisis stage of the pandemic but it was essential in the early days.
3) Social capital builds trust amongst the public
While Australians will always find plenty to criticize about their government, including their poor record on climate change, immigration policy, and reconciliation with the Indigenous populations, but there is always a baseline level of trust in the government due to the fundamental social support all citizens receive. Australians would never think twice about the price tag associated with a Covid-19 test or avoid the emergency room due to fear of bankruptcy. This is all thanks to Australia’s universal health care known as Medicare.
Australia became an early leader in Covid-19 testing when the Peter Doherty Institute in Melbourne was the first laboratory outside China to successfully grow the coronavirus from a patient sample. This provided international laboratories with crucial information to help combat the virus. Australia was among the first countries to implement drive-through COVID-19 testing clinics in March 2020. This meant that Australians could confidently access a Covid-19 test whenever needed through a health system that they trusted. Even when case rates began to lower or hit zero, Australia maintained its vigilance towards testing, nearly 15 million Covid-19 tests have been conducted, equivalent to more than half the country’s population. However countries cannot rely on an accessible health system alone to fight the pandemic. Countries like France have universal healthcare systems and have been unsuccessful in controlling several waves of infection as seen in the chart (Figure 2) below. Accessible healthcare needs to be paired with vigilant public health measures and social support.
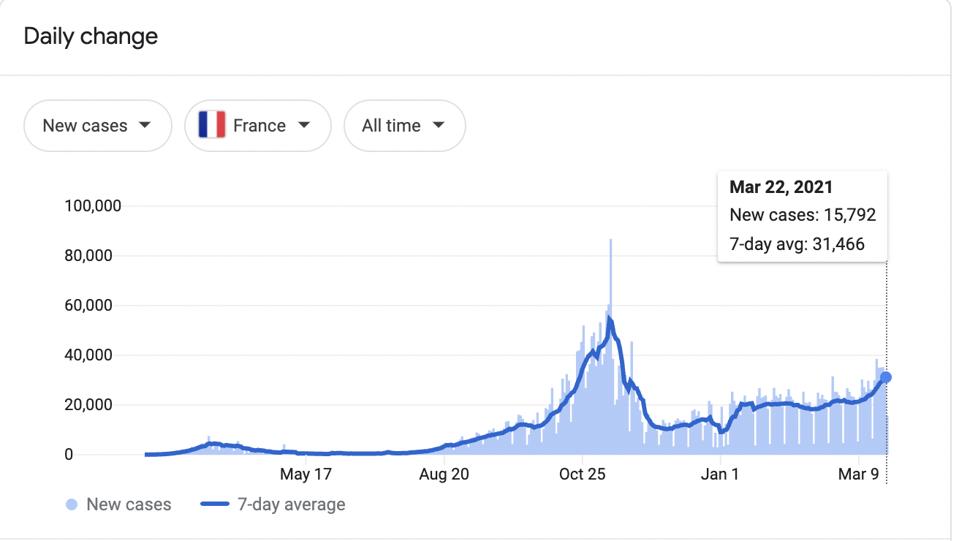
Figure 2: Covid-19 cases in France throughout the pandemic.
JOHN HOPKINS UNIVERSITY VIA GOOGLE
In addition to a strong health system, businesses and employees were provided with swift economic relief. The Jobkeeper program paid the biweekly wages (up to $1500.00) of employees such as hospitality workers who were not able to work during lockdown periods, so they could seamlessly resume work upon the economy reopening. The Jobseeker program provided unemployment benefits. These social supports paired with consistent, clear communication built confidence in the government response and consequently compliance in the public. Australians are known for having a rebellious nature, often describing themselves as “larrikins”. Yet very few Australians protested mask-wearing and restrictions and approval ratings swelled for leaders (even those who were previously unpopular) during even the toughest lockdowns.
4) Meaningfully engage with different communities to find out what they need.
Indigenous Australians have worse health outcomes than other Australians, with a life expectancy of 8 years fewer than non-Indigenous Australians. When Covid-19 struck, they insisted they run their own response and the government listened for once and provided resources. The incredible result was Indigenous Australians were six times less likely to contract Covid-19 and there were zero deaths. Only 148 contracted the disease, and just 15 percent of these people were hospitalized. Remote communities were closed to outsiders, food was supplied to limit travel, and information campaigns were full of Indigenous humor and values. The passion for protecting their elders was a central part of the response. Hopefully, Australia will use the success of this program as a springboard for addressing other Indigenous health outcomes.
Australia’s worst outbreak in the state of Victoria, was partially because migrant communities living in public housing could not access public health information or signage in their own languages. A critical mistake that could have been avoided with better community engagement by the government or local health authorities. This pandemic has taught us all the benefits of engaging with different communities to better understand their needs and or why they aren’t responding to certain policies or initiatives. It’s a lesson we can use not only in the face of a pandemic but in addressing other health disparities as well.
Read the article on Forbes
Originally published on Forbes on March 24, 2021

