The Logic And Practice Of Strict Border Control In Covid-Free Countries
(Posted on Tuesday, May 4, 2021)

A medic collects a swab sample from a traveller at a rapid COVID-19 testing booth in Israel’s Ben Gurion Airport, near Tel Aviv, on April 6, 2021. (Photo by JACK GUEZ / AFP) (Photo by JACK GUEZ/AFP via Getty Images)
AFP VIA GETTY IMAGES
The recent travel bans imposed on travelers from India and Pakistan by governments across the Middle East and in parts of Europe and North America will likely do very little to stem the spread of the new Indian variant. The variant has already reached more than 17 countries, and it has doubtless been unknowingly seeded in dozens of others by infected travelers. It is unfortunate that this far into the pandemic we still have not learned our lesson: reactionary travel bans do not work to prevent the spread of Covid-19. The good news, however, is that we know exactly the border control policies that do work.
A new study out of New Zealand examines the mix of testing and quarantine protocols that are most effective at mitigating the spread of Covid-19 from infected travelers. New Zealand is a great example to learn from as they have kept Covid-19 cases close to zero since May 2020. Since January 1 2021, 397 international arrivals have tested positive for Covid-19 yet none have led to significant outbreaks due to New Zealand’s rigorous quarantine, testing, and tracing policies. The study demonstrates the steps every country should take to control the spread of Covid-19 across borders and within their own countries as well.
While the study doesn’t specifically discuss vaccines, it’s important to note the risk of relying solely on vaccines and vaccine passports to control the pandemic and protect the borders. Vaccines are critically important, but the fully vaccinated border worker at Auckland Airport who tested positive for Covid-19 after cleaning planes from high-risk countries is proof that breakthrough cases can and will happen at the border. And given the recent reports of fake vaccination cards and the possibility of fraud, there’s no guarantee that a person traveling with a vaccine passport is actually vaccinated.
Here are the policies that we know definitively can work:
Comprehensive testing of border workers
Much of the attention on limiting outbreaks at borders is focused on testing travelers to ensure they aren’t infected, but testing shouldn’t just be restricted to visitors alone. Those working in and around border entry points and those who work in quarantine facilities have a high risk of exposure given the environment they work in. According to the New Zealand study, border workers should be tested on a weekly basis, at minimum. Weekly testing increases the chance of detecting an outbreak in the seed case (namely, the border control worker) to greater than 80%, which can significantly limit the size of a potential outbreak. If the seed case is not detected and the first detected case is a secondary contact, perhaps a family member or friend, then the expected outbreak size is much larger.
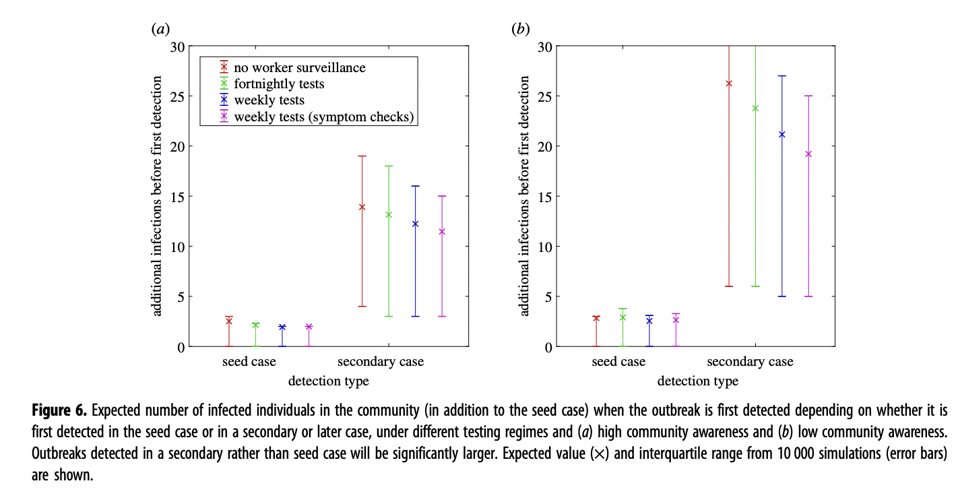
The study is well crafted and accounts for a number of different scenarios. The study authors modeled the potential size of an outbreak based on whether the seed case was detected or whether the first case detected was in a secondary contact, and based on how frequently each group was tested. They also modeled how these outbreaks are affected by levels of “community awareness” of Covid-19 symptoms. Low community awareness is when 50% of infected individuals seek out testing based on symptoms, high community awareness is when this number increases to 100%. Their findings show that If the community awareness is high, the expected outbreak size from one case is likely to be between 11 and 14, the expected size of the outbreak increases to between 19 and 26 if community awareness is low as seen in Figure 6a and 6b in the below chart. This is why it is so critical to detect Covid-19 in the seed cases through regular testing so that quarantining, testing and tracing can occur immediately and the size of the outbreak can be contained.
Figure 6
In addition to the tests, the study authors also recommend symptom checks. Symptom checks that occur 8 days or more after infection increase the probability of a case being identified.
Routine testing protocols and mandatory quarantine for international travelers
Every person should be required to test negative twice for Covid-19 at maximum 36 hours before their travel begins. The first test should be a PCR test, which can show whether a person has an active infection. The second should be an IgM antibody test, which can show whether a person was recently infected and may still be contagious. Some travelers who were recently vaccinated may have a negative PCR test result but a positive antibody test due to the vaccine and not a recent infection. In these cases, an additional antibody test directed at proteins not targeted by the current vaccines would be required.
Upon arriving at their destination all travelers should be tested again with a rapid antigen test or PCR test. We know already that these tests miss cases anywhere from 20% to 100% of the time, depending on when during the course of an infection they’re administered. The authors of the New Zealand study are also skeptical of the accuracy of arrival and destination testing only. In their modeling only approximately 50% of travelers test positive from arrival and departure testing, the low detection rate reflects the high probability that an infected traveler will present a false-negative test during the first 5 days after infection. This also means these individuals who have tested a false negative are likely to be highly infectious when they enter the community. For these reasons, a testing-only policy without quarantine risks too many infected individuals entering the community.
Due to confusion over what constitutes a quarantine and a lack of individual compliance, a managed quarantine facility run through a hotel or purpose-built facility is the best option. Early in the pandemic, Australia instituted a home isolation policy for returned travelers, but after random checks revealed many had no intention of adhering to a home quarantine period they swiftly moved to managed facilities.
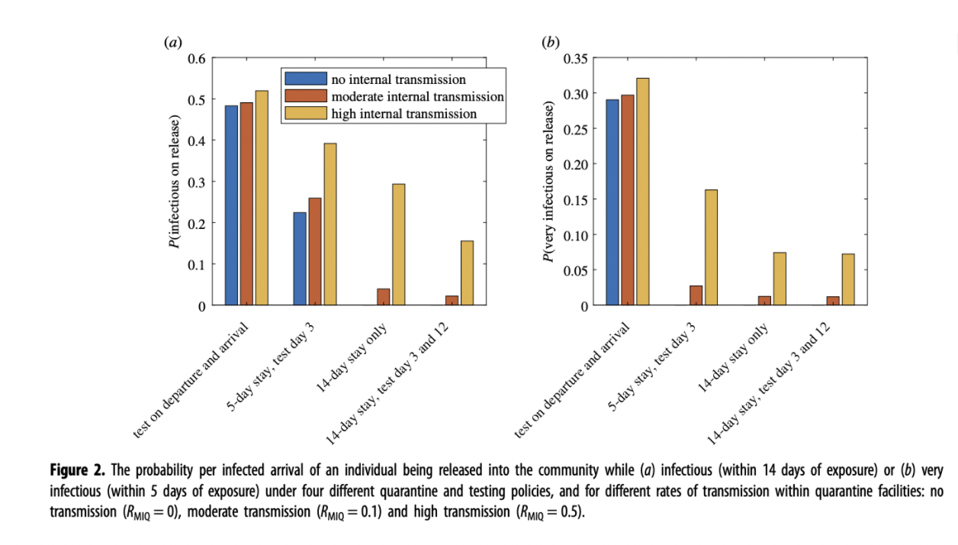
Different countries currently require different quarantine lengths, but the data shows that anything less than 14 days has a substantial impact on the rate of infectious individuals released into the community. The New Zealand study has modeled different quarantine lengths and testing regimes during quarantine with different levels of transmission within facilities. They have also modeled two different scenarios, the percentage of infectious (figure 2a) and highly infectious (figure 2b) individuals released into the community after different border control policies. The varying results are seen in the Figure 2 charts below.
Figure 2
ROYAL SOCIETY PUBLISHING
A 14 day stay in managed isolation with tests on day three and day 12 is proven to be the most effective model in stopping international arrivals from re-introducing COVID-19 into the community. By assuming moderate transmission within quarantine facilities. The risk of an infectious individual being released into the community under this policy is around 2%. The risk of a highly infectious individual (individuals are typically most infectious within 5 days of exposure) leaving quarantine is 1% (figure 2b). If there is high transmission within quarantine facilities due to individuals mixing in facilities, the risk of a highly infectious person entering the community increases to 7%.
If the quarantine period is reduced to a five-day stay with a test on day three, approximately 25% of cases would still be infectious when they entered the community in a low or moderate transmission scenario. If there is high transmission within the quarantine facility, this probability increases to around 38% of infectious and 15% highly infectious individuals entering the community. This would lead to multiple border-related cases in the community every week, making an outbreak inevitable.
Addressing oral-fecal transmission of Covid-19 in quarantine
China has adopted the above policies but has also gone a step further to address the oral-fecal transmission of Covid-19 through quarantine facilities. Those in quarantine in China are required to sanitize their feces and urine with disinfectant tablets in the toilet before flushing.
They are also subjected to anal swabs in addition to regular testing before being released from quarantine. This is because recovering patients have continued to test positive through samples from the lower digestive tract days after nasal and throat swabs came back negative. There is some virological evidence that SARS-CoV-2 can, in fact, replicate in the gut and shed through feces. One study, conducted in Zhejiang, China, discovered viral RNA in the stool of 59 percent of Covid-19 patients tested, remaining at detectable levels for three weeks on average. Another study found that the virus persisted longer in fecal samples than respiratory samples. These interventions may seem extreme, but the rationale behind them isn’t. Evidence not just from the past year, but the original SARS pandemic shows that SARS-CoV-2 infects the intestines and colon and from there spreads to others, traveling from the toilet to the sewer to the water we use and the air we breathe. These strategies have helped China keep Covid-19 cases at close to zero in a population of over 1 billion.
The New Zealand study acknowledges that they did not model for the impact of superspreader style events within quarantine facilities. If confirmed cases are completely isolated then they have found that there is minimal transmission between individuals in quarantine facilities. When designing a quarantine facility it is essential to ensure that guests can stay isolated from one another, even when completing activities such as opening the door to room service or laundry deliveries. In a quarantine hotel in Melbourne, two separate groups of guests staying in adjacent rooms at Melbourne’s Park Royal Hotel tested positive for identical strains of the B.1.1.7 variant. The working assumption was that the viral load of one group of guests was so high that the virus traveled into the hotel hallway when the family opened the door to retrieve food or clean laundry.
Preventing potential interaction between quarantining travelers and employees at the quarantine facilities is also an important element to consider when designing a quarantine policy. Allegations of sexual activity between quarantined travelers and security guards in a quarantine hotel were reported to be one of the factors behind an outbreak in Melbourne, Australia.
For these reasons it is also important to consider the role of aerosol transmission through ventilation systems between rooms in hotel quarantines. Experts in Australia who have encountered this issue, say that we should look to how airflow operates in a Covid ward and replicate that in hotel rooms.
There is likely to be resistance towards implementing a quarantine system for travelers, due to the cost and inconvenience but like most public health measures to prevent the spread Covid-19, the results are clearly the effort.
Read the full article on Forbes
Originally published on Forbes on May 3, 2021