How SARS-CoV-2 Evades And Suppresses The Immune System (Part 4)
(Posted on Tuesday, August 17, 2021)
This is the fourth article in a 15-part series called “Relevance of Immune Suppression by SARS-CoV-2 to Understanding and Controlling the Covid-19 Pandemic,” which will explore an underappreciated but highly significant aspect of SARS-CoV-2 replication. The ability of SARS-CoV-2 to delay, evade, and suppress the immune system has myriad implications for drugs, vaccines, and other aspects of our pandemic response. The first set of pieces in this series are intended for a general audience; the second set, for the medical community; and the third and final set, for biomedical researchers looking for a deeper understanding of variants, how they’re generated, and what we might do to control them. Read part one, part two, and part three.
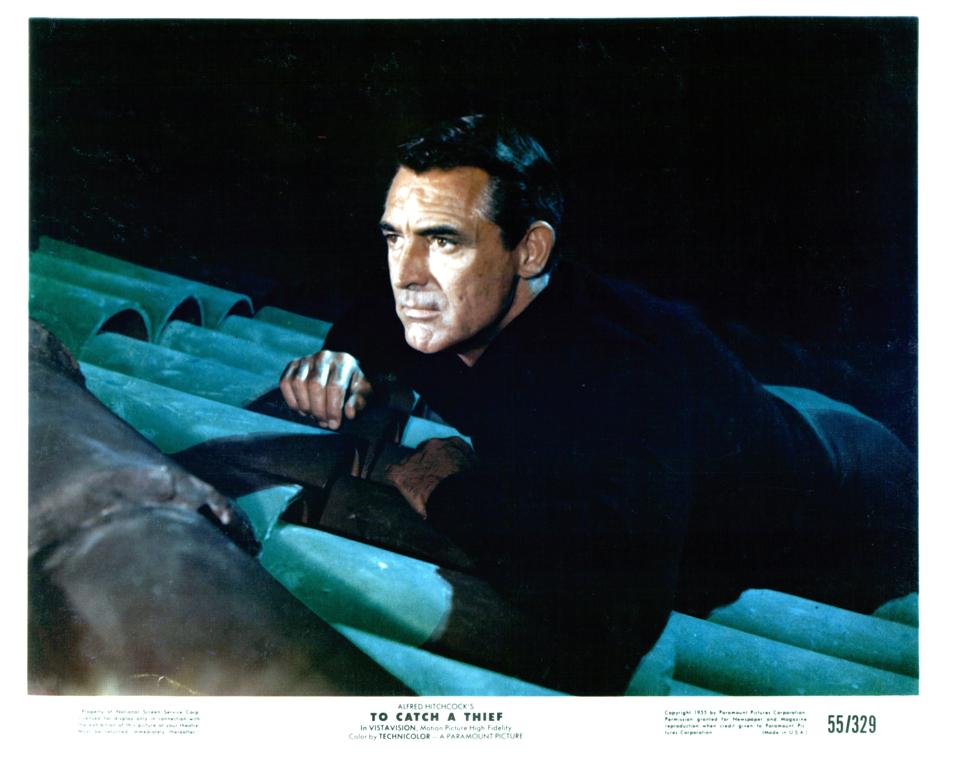
Cary Grant hiding on top of roof in a scene from the film ‘To Catch A Thief’, 1955. (Photo by Paramount/Getty Images)
GETTY IMAGES
What follows is the conclusion of the section of this series written for general audiences. Before this exploration of the immunology of SARS-CoV-2 branches off into more technical detail, I will summarize what we have learned so far using the multilayered analogy of a serial burglar.
Imagine the virus is a burglar not dissimilar to the one Cary Grant plays in Alfred Hitchcock’s 1955 masterpiece To Catch a Thief—a master of slipping in and out of hostile environments undetected. This burglar is so adept at their craft, they can execute a job even at a crowded cocktail soiree.
The first thing the burglar must do upon arriving at the scene is avoid immediate recognition. When he appears at the door, it is as an invited guest, not an intruder—just as SARS-CoV-2, upon entering a human cell, has already changed its exterior so as to evade immune detection.

(Original Caption) Grace Kelly and Cary Grant in ‘To Catch a Thief’ by Alfred Hitchcock. (Photo by Paramount Pictures/Sunset Boulevard/Corbis via Getty Images)
CORBIS VIA GETTY IMAGESSecond on the burglar’s agenda is surreptitiously anesthetizing the guests. The virus, as we’ll see in upcoming pieces in this series, has an impressive capacity for arresting the many checkpoints the cell normally has in place to impede infection.
Next the burglar must disarm the security system. The equivalent of this for SARS-CoV-2 occurs when the virus silences the many signals an infected cell typically sends to alert nearby cells to the presence of an intruder.
Last but not least, to top it all off, the burglar breaks the fire alarm and starts a fire to cover his tracks and divert attention away from himself before moving on to the next function. The fire stands in for the immune dysregulation the body can experience if a Covid-19 infection progresses to more critical stages of illness, potentially ending in death.
However facile this analogy may seem, it bears a close resemblance to what actually occurs when SARS-CoV-2 imposes itself upon a human host. I will now describe the mechanics of the first part of this process, when the virus disarms our first line of immune defense.
Evasion of innate immunity
When an invading pathogen activates the body’s extensive, interferon-led warning system, it triggers three types of immune response. The first is the innate immune response. This line of defense goes on the offensive when the identity and purpose of a pathogen is unknown. The second is the adaptive immune response, which is composed of antibodies and T cells that recognize and attack specific pathogens. The third and final wave is the T and B cell memory response.
Innate immunity involves proteins known as pattern-recognition receptors that, over the course of evolution, have been hard-wired to identify pathogen-associated molecular patterns or PAMPs. Commonly found in many pathogens, recognition of these molecules allows the body to respond immediately to invaders old and new. Some of the better-known PAMPs include bacterial lipopolysaccharides, acids, bacterial DNA, and both single- and double-stranded RNA. Activation of these pathways is also necessary to trigger the adaptive immune response.
Is innate immune suppression observed in newly infected Covid-19 patients? The answer, according to lab studies of cultured virus and Covid-19 patients, appears to be yes. One group of researchers conducted an exhaustive survey of proteins and peptides excreted in the urine of uninfected and infected but asymptomatic or mildly ill patients. Many proteins involved in the innate immune response were markedly downregulated, while proteins characteristic of a hyperimmune state were present in patients with severe disease. Another study monitored the expression of immune-related genes in the respiratory cells of infected patients. They found very few changes in the activation of innate immune response genes within the first 24 hours post-infection.
Together, these experiments demonstrate the ability of SARS-CoV-2 to suppress the immune response in the first few days following infection. Remember, the first obvious symptoms of infection are the consequence of the immune reaction to the virus, not to virus-induced damage itself.
My next piece for this series will be the first of several that explores the virus’ mechanisms of immune suppression in depth. We’ll begin with the specialized compartment SARS-CoV-2 erects to hide its replication activities from the rest of the cell.
Originally published on Forbes (August 17, 2021)

