Study Shows Unvaccinated People Are At Increased Risk Of Infecting The Vaccinated
(Posted on Friday, May 6, 2022)
A new modeling study published in the Canadian Medical Association Journal demonstrates that unvaccinated people threaten the safety of the vaccinated even when SARS-CoV-2 vaccination rates are high.
Researchers used a simple compartmental model of respiratory viral disease to explore the effect of mixing between unvaccinated and vaccinated people. People were represented as residing in 3 possible compartments including susceptible to infection, infected and infectious, and recovered from infection with immunity. Those compartments were divided to reflect the two connected subpopulations: vaccinated and unvaccinated people.
The researchers simulated mixing of like-with-like populations in which people have exclusive contact with others of the same vaccination status as well as random mixing between different groups. When unvaccinated mixed with unvaccinated, the risk to vaccinated people was lower. When vaccinated and unvaccinated people mixed, a substantial number of new infections would occur in vaccinated people, even in scenarios where vaccination rates were high. Cumulative infection rates among vaccinated people were highest (15%) with random mixing. Unvaccinated participants exhibited a disproportionate contribution to infection risk following contact count adjustment.
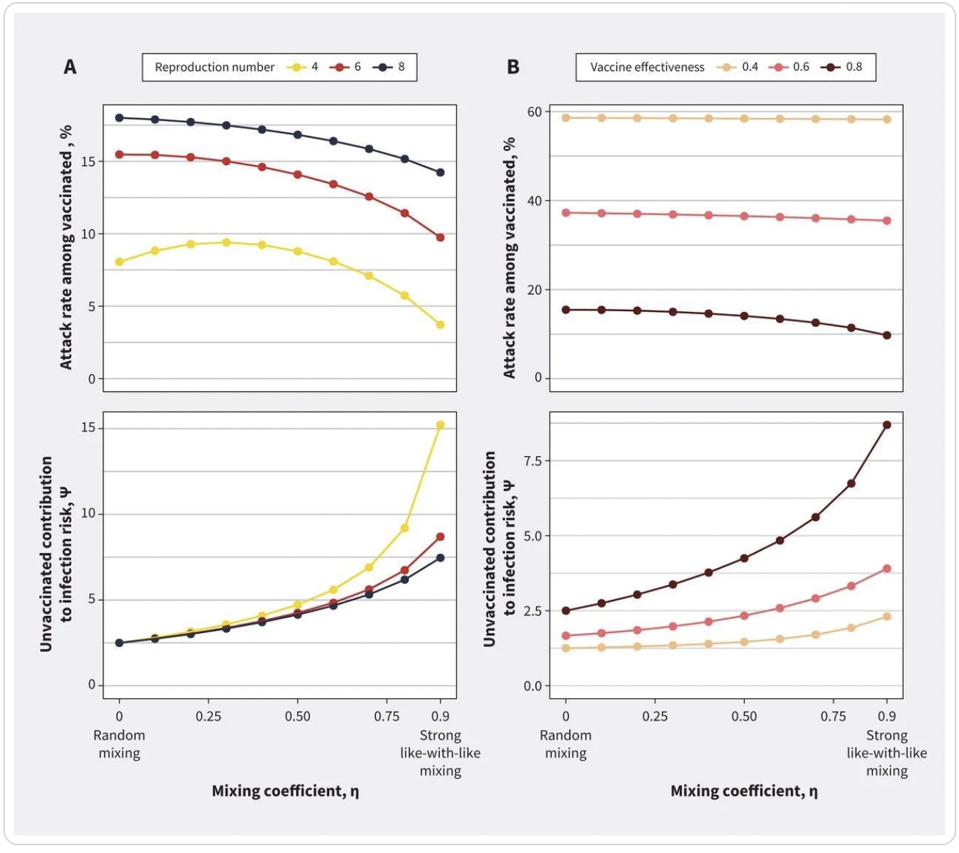
Impact of mixing between vaccinated and unvaccinated subpopulations on contribution to risk and final epidemic size for (A) varying reproduction numbers and (B) vaccine effectiveness. Both panels show the impact of increasing like-with-like mixing on
IMPACT OF POPULATION MIXING BETWEEN VACCINATED AND UNVACCINATED SUBPOPULATIONS ON INFECTIOUS DISEASE DYNAMICS: IMPLICATIONS FOR SARS-COV-2 TRANSMISSION. FISMAN ET AL. 2022
The findings remained stable even when they modeled lower levels of vaccine effectiveness for the prevention of infection, such as in those who have not received a booster dose or with new SARS-CoV-2 variants. The lower-bound estimate for vaccine effectiveness (40%) reflected uncertainty about the emerging Omicron variant at the time. In contrast, the upper-bound estimate for vaccine effectiveness (80%) reflected the higher effectiveness seen with the Delta variant.
The authors acknowledge that there are some limitations to the simplicity of their model. Vaccine effectiveness against infection was modeled but not the additional benefits of vaccination for preventing severe illness and the impact of vaccines on prevention of forward transmission by vaccinated but infected individuals. However, the simplicity of the modeling does unequivocally demonstrate the infection risk of the unvaccinated.
Those opposed to vaccinations and vaccine mandates often argue that it is a matter of personal choice or individual rights. However, this study reinforces the fact that an individualistic or personal responsibility approach to Covid-19 will result in poor pandemic control. The actions of the unvaccinated impact the broader population.
A report from Frontiers in Public Health found that the more “individualistic” a country was, the higher the instance of Covid cases and mortalities. The report also found that the more individualistic participants were, the higher the chances they would not adhere to epidemic prevention measures.
According to the CDC, only 66.1% of the U.S. population has received two doses of the Covid-19 vaccine and even fewer have received boosters. We need better more nuanced messaging on why vaccination against Covid-19 is so critical. The original messaging that Covid-19 vaccines would prevent all instances of infection was unrealistic and not in keeping with results from other vaccines. But vaccines do not need to prevent infection to be highly effective. The Salk inactivated virus Polio vaccine for example does not prevent infection or transmission but has been responsible for the eradication of Polio in the US and in many other countries worldwide.
Vaccination also radically reduces the chance of severe disease, death, and hospitalization. This reduces the burden on our healthcare systems. If hospitals are overwhelmed with Covid cases it affects the standard of care for all health issues. No person or population is safe from the scourges of Covid-19 until we all are.
Public health policy and regulation in the past have been developed around behaviors that create health risks for the community, as well as individuals. For example, if we have public health statutes that limit indoor smoking and driving under the influence of alcohol and drugs, it may be time to consider vaccination against Covid-19 in the same regard.
Originally published on Forbes on May 6, 2022

