Should You Get Vaccinated For Covid-19? Yes. Will It Protect You From Long Covid? Probably Not.
(Posted on Monday, July 18, 2022)
Lenox Hill Hospital Chair of Emergency Medicine Yves Duroseau receives the COVID-19 vaccine from Doctor Michelle Chester at Long Island Jewish Medical Center on December 14, 2020 (Photo by Scott Heins/Getty Images)
GETTY IMAGES
The United States is amidst a new Covid-19 wave. BA.2.12.1, the previous variant of concern, has been outcompeted by highly transmissible Omicron sub variants BA.4 and BA.5.
BA.4 and 5 contribute 16 and 65 percent respectively to the 110,000+ Covid-19 cases seen daily—a conservative estimate considering at-home testing results are not included. And infection rates are forecasted to rise. These two variants are more likely than BA.2.12.1 to lead to vaccine breakthrough infections. As a result, even persons up-to-date on vaccines or recently recovered from Covid-19 are susceptible to reinfection.
It is unknown if BA.4/5 cause less severity of disease than their predecessors. What is known is that, while vaccination does not protect against infection, it seems to successfully prevent hospitalizations and deaths. Latest CDC statistics show a 3.1% uptick in hospitalization rates, averaging over 5,700 hospitalizations a week. The current 7-day moving average of new deaths (273) actually decreased 20.9% from the previous week. Although this level of hospitalization and death is still unacceptable, it is comparatively modest to prior waves. With 78.4% of the US population protected with at least 1 dose of a Covid-19 vaccine, 67% fully vaccinated, and 47.9% boosted, the wide-spread adoption of vaccines has likely dampened the increase in observed rates.
Vaccination + Long Covid
The consequences for Covid-19 may appear mild, but each infection has the risk of developing serious post Covid complications, otherwise known as Long Covid. There are several circulating definitions for Long Covid. In my book A Family Guide to Long Covid: Questions and Answers, I define Long Covid broadly to highlight several long-term complications, such as organ damage caused by acute Covid-19. More generally, it is characterized by a heterogeneous collection of symptoms which arise after SARS-CoV-2 infection has cleared and linger for a long time. Fatigue, shortness of breath, and brain fog are commonly reported symptoms which, depending on severity, can intensely disrupt daily life for months (or more).
Current covid-19 vaccines prevent hospitalization and death—do they also prevent Long Covid? A study published in The Journal of the American Medical Association confirms an existing observation: that vaccination provides little protection against developing Long Covid.
This study observed 739 Italian health care workers who had Covid-19 but were not hospitalized for it. 229 individuals from this group had Long Covid. The authors defined Long Covid as any SARS-CoV-2-related symptom which lasted more than four weeks. Individuals with asymptomatic Covid-19 were included in 739 member cohort although they could not, by the study’s standards, develop Long Covid (note that asymptomatic cases have been observed to lead to Long Covid beyond the scope of this study).
All health care workers completed surveys—which included a list of SARS-CoV-2 symptoms and their duration along with vaccination status—and were tested every one to two weeks for positive SARS-CoV-2 results. Some mentioned symptoms are fatigue, loss of concentration, shortness of breath, and problems sleeping.
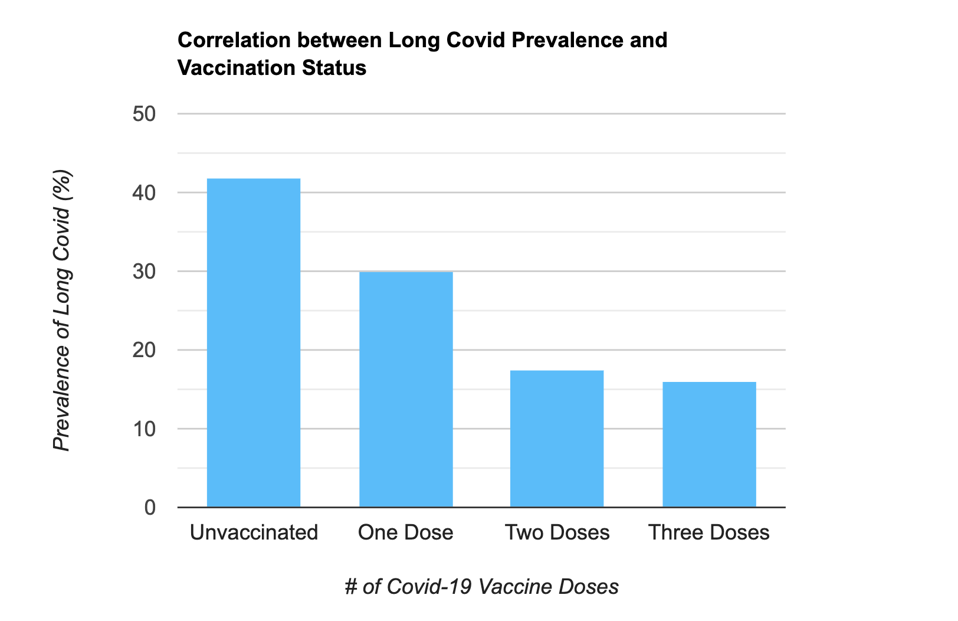
The correlation between Long Covid prevalence and vaccination status, as referenced by “Association Between BNT162b2 Vaccination and Long COVID After Infections Not Requiring Hospitalization in Health Care Workers. JAMA”
ACCESS HEALTH INTERNATIONAL
From the survey results, the authors found that the number of vaccine doses was associated with lower Long Covid prevalence. Unvaccinated health care workers reported a 41.8% incidence of Long Covid; those with one dose reported 30%. Patients with two doses reported a 17.4% incidence, and those with three reported 16%. According to these results, vaccines can only reduce one’s chances of getting Long Covid by about 24-5% at best, and only if the individual is fully vaccinated and/or boosted. All administered doses in this study were of Pfizer’s BNT162b2 vaccine.
This data supplements findings by a study of US veterans which saw a 15% reduction of Long Covid after vaccination. The scale of the veteran’s study was much larger. However, the age skewed towards older persons and included a low number of women (only 8-10%). This is an important distinction, as women are more likely to develop Long Covid symptoms after infection compared to men.
The two studies suggest that vaccination can reduce one’s chances of Long Covid, but the protection gained is not strong. Individuals with at least two vaccine doses may benefit slightly from this correlation.
Is it worth getting vaccinated?
Ultimately, should you still get vaccinated and boosted? Generally, yes. Vaccination is essential to reducing one’s chances of hospitalization and death. However, if you’re looking to get boosted to avoid Long Covid, it’s best to temper expectations. Recent studies suggest that current Covid-19 vaccines offer meager protection from Long Covid. The best means of avoiding Long Covid will be to use preventative measures as needed—such as mask wearing and social distancing—to prevent getting Covid-19 to begin with.

