Mild Covid Inflicts Paradoxical Brain Damage: Detected By Imaging But Not By Neuropsychological Assessment
(Posted on Monday, July 25, 2022)
Brain fog—or difficulty thinking or concentrating—plagues many who recover from Covid-19. Along with fatigue, lightheadedness when standing, and trouble sleeping, Covid-caused neurological symptoms may linger for weeks to months at a time. These ailments can develop even after asymptomatic and mild cases of Covid-19, raising the suspicion that even moderate acute Covid-19 could impact the brain. Here we describe a recent study by Petersen et al. which examines the correlation between SARS-CoV-2 infection and the brain. While the authors identified SARS-CoV-2 damage to the white matter of the brain, the structural changes paradoxically were not associated with worse neuropsychiatric scores.
Study Design
Petersen et al. investigated the possible correlation between mild to moderate SARS-CoV-2 infection and its impacts on the brain. The team studied 223 non-vaccinated participants around 289 days after recovering from mild to moderate Covid-19. Seven participants were asymptomatic; 126 had mild symptoms; sixty seven had moderate Covid-19 but were not hospitalized; and eighteen were hospitalized but did not receive intensive care treatment. Polymerase chain reaction tests (PCR), obtained between March and December 2020, confirmed SARS-CoV-2 exposure. A healthy control group—examined prior to the Covid-19 pandemic—was matched for age, sex, years of education and cardiovascular risk factors and underwent the same process.
The authors sought eleven signs of neurodegeneration, atrophy, inflammation, blood vessel damage and cellular disruption through magnetic resonance imaging (MRI) scans. The imaging markers demonstrate alterations in the cortical gray and white matter of the brain in vivo. For reference, the outermost layer of the brain is composed of gray matter and is otherwise known as the cerebral cortex; white matter lies directly underneath. Notably, Petersen et al. used conventional diffusion tensor imaging (DTI) markers to non-invasively reveal information on white matter microstructures.
The individuals also received clinical and neuropsychological assessment to detect any issues with cognitive function or psychosocial burden. A trained study nurse conducted four subtests of the Alzheimer’s Disease Neuropsychological Assessment Battery (CERAD-Plus) and a clock drawing test; these examinations assess neuropsychological functions such as attention, language, memory, and psychomotor function. A patient health questionnaire screened for anxiety and depression. Common complaints of Covid and Long Covid were noted. This includes, but is not limited to, headache, dizziness, fatigue, and sleep disturbances.
Results
The researchers did not identify any significant changes in the mean thickness of the whole brain (cortical thickness) or any visually apparent vascular lesions. The nominal increase seen in peak width of skeletonized mean diffusivity (PSMD), a calculated marker of cerebral small vessel disease, did not survive statistical correction. These results contrast preliminary evidence from the UK biobank which associated cortical thickness reduction to neurocognitive decline in former Covid-19 patients.
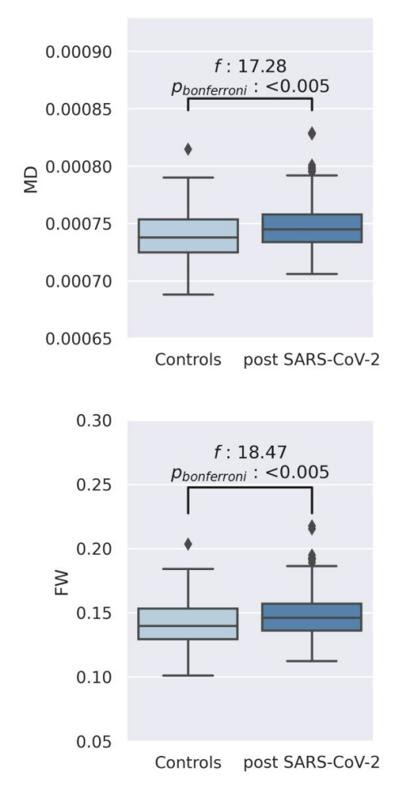
FIGURE 1: Boxplots depict the comparison of mean diffusivity (and free-water averaged across white matter skeletons between post-SARS-CoV-2 individuals and matched controls
PETERSEN ET AL, BRAIN IMAGING AND NEUROPSYCHOLOGICAL ASSESSMENT OF INDIVIDUALS RECOVERED FROM MILD TO MODERATE SARS-COV-2 INFECTION
Petersen et al. did find that those who recovered from Covid-19 displayed higher average free-water (FW) and mean diffusivity (MD) in the white matter of the brain than healthy controls. Free-water denotes the extracellular fluid found between the brain’s tissues, and mean diffusivity describes the magnitude of water diffusion within brain tissue. Larger free-water and mean diffusivity measurements usually suggest neuroinflammation, and have been associated with normal aging and disorders such as schizophrenia.
This small but significant change is demonstrated in Figure 1, where post SARS-CoV-2 participants (dark blue) have a higher standard deviation than the controls (light blue) for both measurements. The free-water mean standard deviation is 0.148 ± 0.018 for post SARS-CoV-2 participants versus 0.142 ± 0.017 for controls; mean diffusivity is 0.747 ± 0.021 vs. 0.740 ± 0.020 respectively. Also seen in Figure 1, the p value for both measurements is less than 0.05 and thus is statistically significant.
Consequences on Neuropsychological Results
Higher free-water and mean diffusivity in white matter suggests even mild to moderate Covid-19 survivors have more neuroinflammation than healthy controls. Brain white matter governs information transfer. Although damage to this deeper section of the brain can impair problem solving, memory, focus and mobility, the observed microstructural changes in white matter were not associated with decreased cognitive functioning in Covid-19 recoverees. Post-SARS-CoV-2 participants actually showed better results for verbal fluency, early dementia and early Alziehmer’s, but the research team states that no significant group differences remained after test scores were statistically corrected for multiple comparisons.
The authors suspect that the increase in free-water and mean diffusivity could be an indirect sign of a prolonged neuroinflammatory reaction—specifically endothelial dysfunction followed by vascular leakage—to SARS-CoV-2 infection. They also note that other possible mechanisms still need to be considered.
Further Implications
The study concluded that small changes in the brain’s white matter water level can persist within one year of recovering from Covid-19. In the short-term, this change did not translate to any significant cognitive deficits for this group of participants. Important to consider is a virus’s ability to cause damage which remains undetectable for years; the influenza virus, for example, can cause Parkinson’s disease in rare instances. Additional longitudinal studies are therefore required to understand if longer term ramifications also exist for SARS-CoV-2. More information on Covid-19 and the brain can be found in this article: Head in the Clouds: Living with Covid-19.