A New Hope For Osteoarthritis Treatment And Prevention (Part 2)
(Posted on Sunday, May 21, 2023)
In this second installment of our stories on osteoarthritis, we discuss a new approach for treatment and cure. Both stories are part of our series on regenerative medicine. We define regenerative medicine as any medical modality which restores normal function—whether damaged by disease, injured by trauma, disadvantaged by birth or worn by time. For more on this topic, visit www.williamhaseltine.com and search regenerative medicine.

New research in osteoarthritis leaves hope for an injection that prevents or restores joint damage.
GETTY
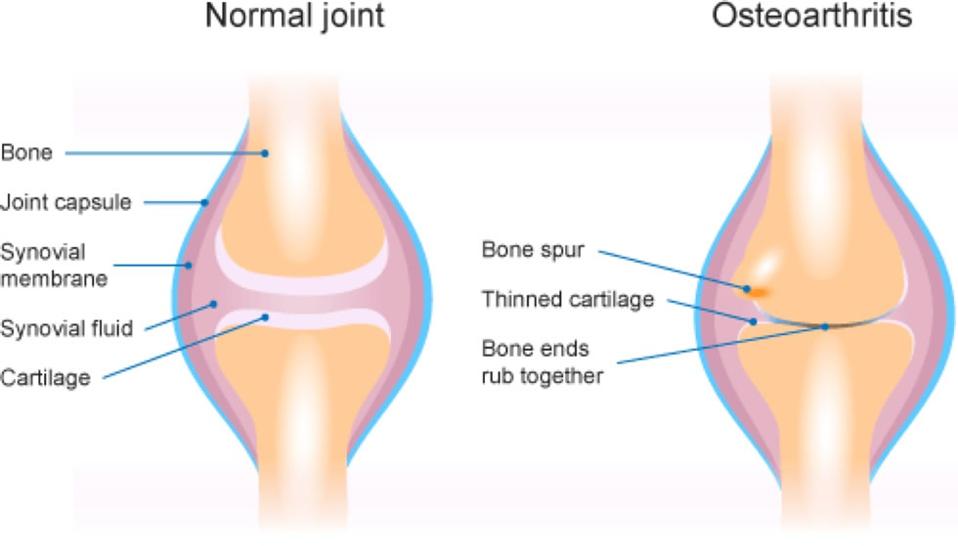
Osteoarthritis is a common degenerative joint disease that results from aging or injury. Although the swelling, stiffness and pain in the joints can impair daily life or even lead to disability, treatment options are limited. A recent study in Science Advances provides insight into the role of an imbalance in repair and inflammation processes in the diseased joint. This new understanding offers a path toward treatment and possibly a cure.
Addressing the Synovial Fluid
In their study, Bolander and colleagues at the Wake Forest Institute of Regenerative Medicine discovered that synovial cells in arthritic joints have the capacity to rebuild damaged cartilage, but that arthritic synovial fluid prevents the cells from doing so.
What is in the arthritic synovial fluid that prohibits regeneration? Compared to healthy synovial fluid, it contains higher levels of pro-inflammatory proteins including interleukin-17A and interleukin-6, and lower levels of pro-regenerative and anti-inflammatory cytokines such interleukin-2, interleukin-4 and interleukin-10. This aligns with previous literature. In theory, then, a cell treatment could be injected into the arthritic joint to help restore a favorable balance of inflammatory and degenerative conditions in the diseased joint.
Developing the Cell Treatment
The experimental treatment required two types of cells: cartilage-activated T cells, derived from the blood and spleen; and mesenchymal stromal cells—progenitor cells taken from adipose tissue. The former will eventually direct the latter to differentiate into cartilage.
The initial step in the healing process is to create T cells capable of stimulating cartilage regeneration. The T cells originate from a large pool of immune cells called mononuclear cells derived from the patients’ own blood. Exposing the mononuclear cells to an attractant and inhibitors for pro-inflammatory cells activated the T cells present, creating a source of cartilage-activated T cells. Cartilage-activated T cells produce high levels of pro-regenerative cytokines and cartilage-inducing factors.
During this time, the progenitor cells are expanded in a separate growth medium. Activated T cells are added to this medium at a 4:1 ratio. The T cells and stromal cells co-culture together for 24 hours, a process which primes the stromal cells for cartilage regeneration. The final injection, made from this mixture of immune and primed cells, is finally administered into the diseased joint.
This design should counter the inflammatory factors in the joint and provide a much needed regenerative boost. Ideally, the T cells would encourage the injected progenitor cells, and even recruit cartilage cells already in the joint, to repair the local tissue damage.
FIGURE 1: Comparison between a normal joint and a joint with osteoarthritis. In this study, the authors hypothesize that the synovial fluid surrounding the joint prevents injured cartilage from healing. This, in turn, leads to fibrosis and osteoarthritis.
COASTAL PODIATRY
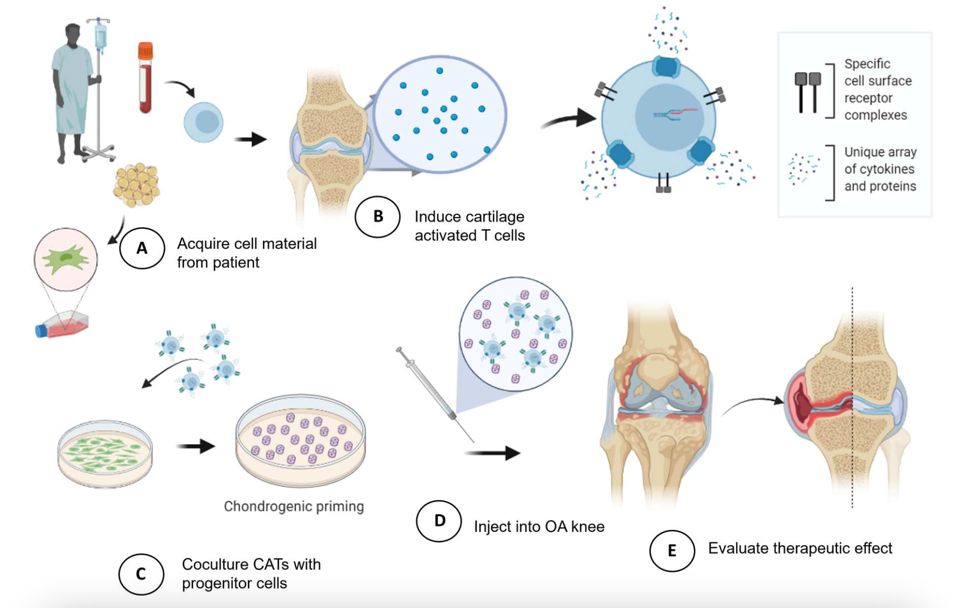
FIGURE 2: Overview of osteoarthritis (OA) treatment development. A) Two types of cells are isolated and multiplied: adipose mesenchymal stromal cells (aMSCs) and mononuclear cells (MNCs), derived from blood or spleen. B) The mononuclear cells are stimulated to become cartilage activated T cells (CATs). The cytokines and proteins expressed by the T cells direct the stromal cells towards cartilage tissue development. C) The activated T cells are then added to the stromal cells, conditioning them to differentiate into cartilage cells. D) The cells are injected into the knee of patients with severe osteoarthritis E) to see if the treatment improves their condition.
BOLANDER ET AL., 2023.
Restored Joint Balance in Rat Models
The treatment was first tested in rat models of osteoarthritis.. Signs of cartilage deterioration could be seen one week after disease induction. Three weeks later, the rats were injected with either plain mesenchymal stromal cells, cartilage-activated T cells.
The mesenchymal stromal cells on their own had little effect. The activated T cells alone were promising, but still limited. The best results were found in rats that received a combination of activated T cells and the mesenchymal cells. The combined treatment resulted in near complete restoration of the injured joint to normal function. The thickness and composition of the synovial membrane was also restored to near normal function.
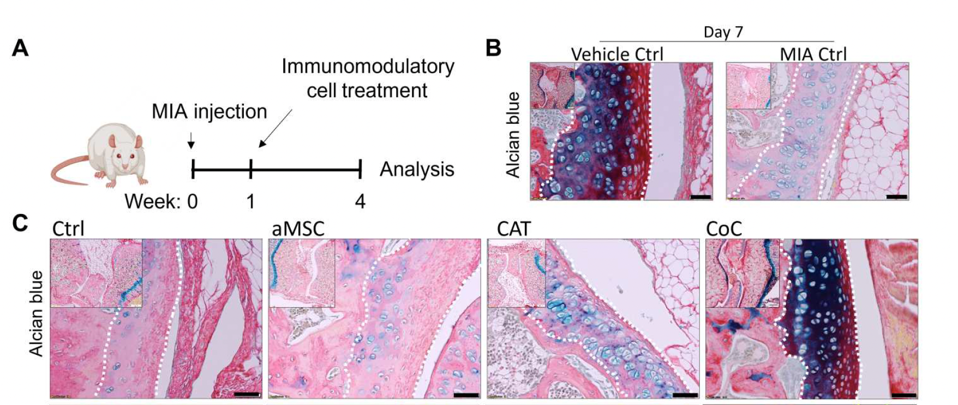
FIGURE 3: A) The researchers chemically induced osteoarthritis (MIA ctrl) in rats. B) On the left, the vehicle control control (ctrl) did not show any signs of cartilage degeneration; on the right, degeneration was evident in the chemically induced mice. C) The team used collagen staining to analyze the impact of adipose-derived mesenchymal stromal cells (aMSC), cartilage-activated T cells (CATs) and their combined cell treatment (CoC) on cartilage regeneration. The joints in the arthritic mice with the combined cell treatment resemble the joints of the mice without osteoarthritis.
BOLANDER ET AL., 2023.
Human Trials
Bolander et al. described the effect of treatment of nine patients with severe osteoarthritis with a mixture of autologous activated T cells and mesenchymal cells. Osteoarthritis severity was measured by three factors:
- Pain, reduced quality of life, and reduced function in daily life and sports
- X-ray appearance
- MRI analysis
All patients received either one of two cell treatment injections into the knee. They had a follow-up one year later to evaluate any changes in their condition.
Most patients experienced a significant improvement in quality of life; pain and symptoms improved, as did function in daily life and sport. Most fascinatingly, the injection seemed to restore function in some very severe cases of osteoarthritis and injury.
Prior to the treatment, one athlete was previously prescribed a combination of rest, therapy, pain medication and steroid injections to preserve their knee—this regime failed. Another patient injured their anterior cruciate ligament, or ACL. In both cases, the treatment significantly restored joint cartilage and the joint’s overall condition; the athlete experienced less swelling at the knee, and the bones in the other patient did not rub together as fiercely.
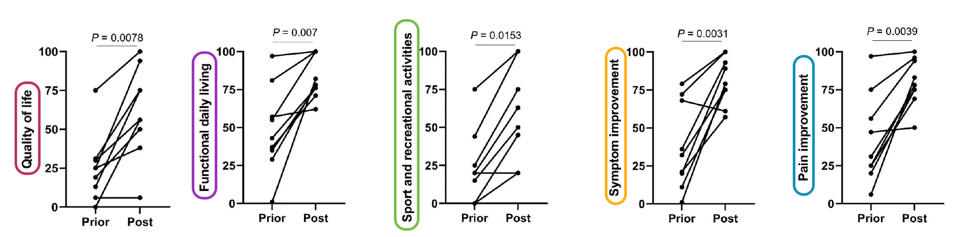
FIGURE 5: Scores prior to the injection(s) versus one year post injection, according to the Knee Injury and Osteoarthritis Outcome Score. The charts reflect, on average, improved scoring for quality of life, functional daily living, sport and recreational activities, symptom improvement and pain improvement.
BOLANDER ET AL., 2023.
Future Implications
Bolander et al. offer an explanation for why joint cell function is impaired, and suggest a possible remedy. They show that a selected mixture of the patient’s own cells, if grown together with the correct mixture of stimulating and inhibiting factors, has the potential to regenerate cartilage and restore the diseased joint to normal function. The limitation of this study is the small number of patients enrolled in the study. Nonetheless, it may be the first truly positive step on the long road to treatment and cure of this widely prevalent and disabling disease.