Kidney Function Successfully Modeled In Cell Culture
(Posted on Wednesday, July 19, 2023)
Originally published on Forbes on July 19, 2023.

3D illustration of human kidneys with cross-section GETTY
Scientists have made a remarkable breakthrough in kidney research. In a paper published in the journal Biology Communications, a team of researchers at Kyoto University led by Ramin Sadeghian present an innovative approach to building miniature kidney models that closely resemble the structure and function of full-sized human kidneys.
The miniature kidney models combine two common approaches for modeling human organs: organoids and microfluidic chips. By combining these approaches, the researchers were able to enhance the accuracy of their kidney model, marking a significant step towards creating miniature kidneys that could be used for medical research and drug development.
What are organoids?
Organoids are created from stem cells. Stem cells are unique in that they have the remarkable ability to develop into almost any cell type. When these cells are provided with the correct environmental and chemical cues, they can be coaxed into interacting with each other and forming human tissue, including tissue that makes up our vital organs like the kidneys.
The model presented by the Kyoto University researchers overcomes previous difficulties in kidney organoid research by incorporating a more accurate model of a structure called the proximal tubule. The proximal tubule is a major site of nutrient absorption and waste elimination in the kidneys.
The benefits of microfluidic chips
An alternative approach to modeling organs is by using microfluidic chips. Microfluidic chips consist of materials like glass and silicon with microscopic channels engraved into them. These microscopic channels contain small amounts of fluids. This allows researchers to have greater control over the environment that cells grow in by easily manipulating the pressure and flow of liquids inside the channels.
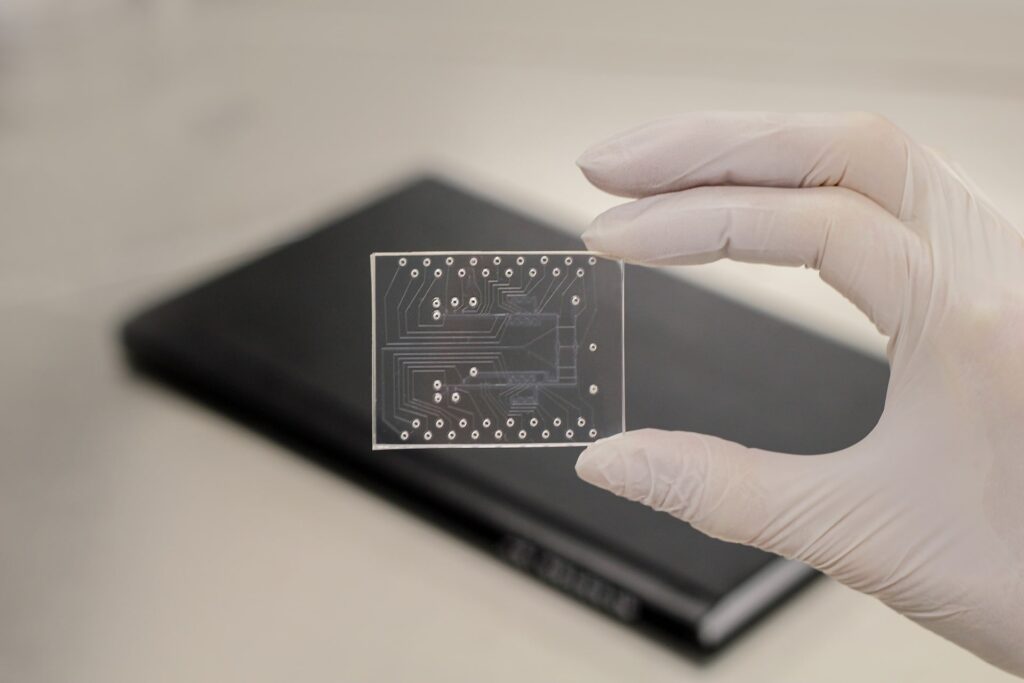
Figure 1: Microfluidic chips are materials with microscopic channels engraved into their surface.
UFLUIDIX, URL: HTTPS://WWW.UFLUIDIX.COM/RESOURCES/DEFINITIONS/
Proximal tubule cells have been generated and used directly in microfluidic chips as a model of the kidneys. However, these models are not the most accurate because they do not represent many of the complex cellular interactions between proximal tubule cells and other kidney cells.
A combined approach
The Kyoto University researchers speculated that by combining organoids and microfluidic chips, they could model the function of the proximal tubule while incorporating important cellular interactions that previous models overlooked.
To begin the process, stem cells were coaxed into forming basic kidney organoids through a series of precise chemical and environmental manipulations. After allowing the kidney organoids to mature, researchers added fluorescent biomarkers to their organoids to confirm that the miniature kidneys contained the correct composition of kidney cell types. This step also allowed them to determine that the organoids were composed of roughly 20-30% proximal tubule cells.
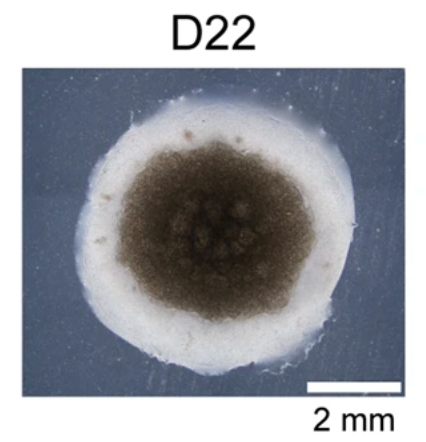
Figure 2: Kidney organoid growth after 22 days.
SADEGHIAN ET AL., COMMUNICATIONS BIOLOGY (2023), DOI: 10.1038/S42003-023-04862-7
From there, the team broke down the organoid and separated the proximal tubule cells. The researchers hoped that by allowing the proximal tubule cells to first grow in an organoid environment and then be transferred to a microfluidic chip that the cells would continue to behave in the way that they did when cultured with other kidney cell types. This would lead to a more accurate “proximal tubule on a chip” model.
After culturing the proximal tubule cells within a microfluidic chip, the researchers noticed that the cells began to aggregate to form tiny spheres within the microfluidic chip’s channels. Despite this behavior, fluorescent stains confirmed that the spheres still contained an abundance of proximal tubule proteins, suggesting that the cells were developing successfully within the chip.
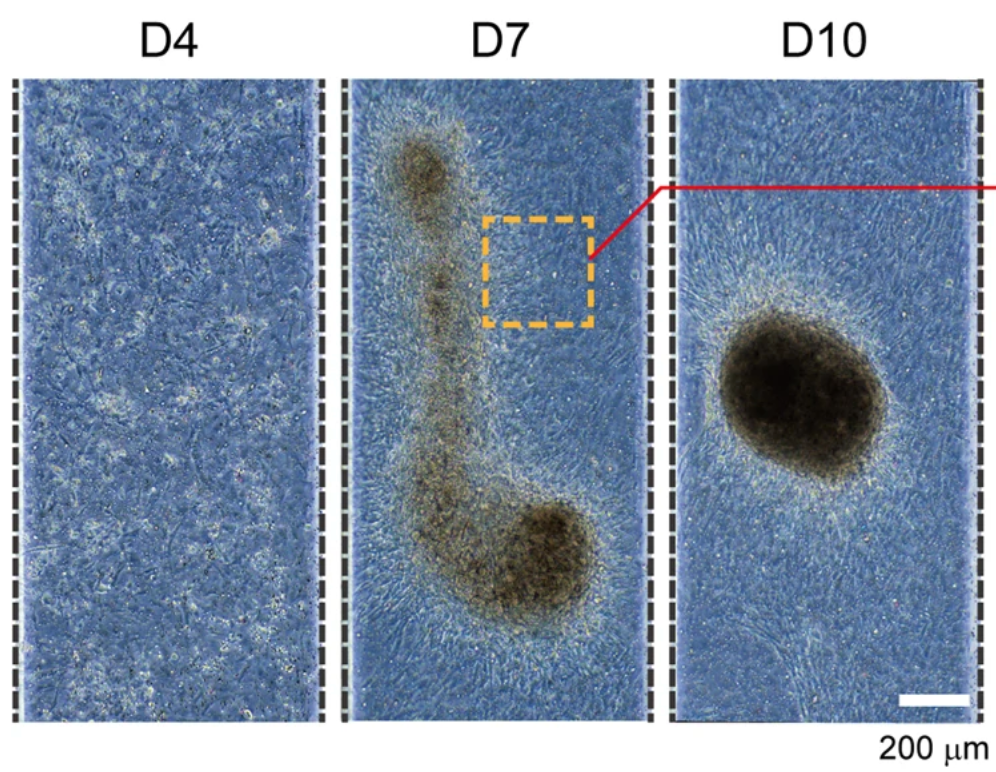
Figure 3: Proximal tubule cells formed spheres within the microfluidic channels.
SADEGHIAN ET AL., COMMUNICATIONS BIOLOGY (2023), DOI: 10.1038/S42003-023-04862-7
To coax the proximal tubule cells into forming a layer of kidney tissue within the microfluidic chip, the researchers added a secondary cell type to their culture. These cells were immortalized renal proximal tubule epithelial cells.
Immortalized cells have been mutated so that they continue dividing and producing new cells indefinitely. Epithelial cells form the surface of kidney tissue. Once these cells were co-cultured with the proximal tubule cells, the resulting tissue flattened out within the chip, forming model kidney tissue that could be used for experimentation.
Several tests determined that the model kidney tissue produced proteins that were in line with actual human kidney cells. Additionally, the model kidney had a greater filtration capacity than previous models.
Finally, to simulate the environment of the human body, the team assessed how their model kidney performed when placed in a dynamic fluid environment. The researchers used a pump to push fluids through the microfluidic device in a pulsating manner—much like the human body pumps liquids through the kidney. As expected, the dynamic fluid environment improved the structure and function of cells in the model.
This paper marks a significant milestone in kidney research. By integrating immortalized cells with kidney organoids, scientists have created miniature kidney models that more accurately replicate the crucial functions of the proximal tubule. This progress offers opportunities for understanding kidney diseases and accelerating drug discovery. As researchers continue to improve these remarkable miniature organs, we can anticipate a future where kidney diseases are better understood and treated.

