Reclaim Your Sight: How Minimally Invasive Glaucoma Surgery and Microshunts are Changing the Game
(Posted on Wednesday, November 15, 2023)

Rear view of male surgeon wearing surgical mask in operation theater at hospital
This article was published on Forbes on 11/9/2023.
This story is part of a series on the current progression in Regenerative Medicine. This piece is part of a series dedicated to the eye and improvements in restoring vision.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
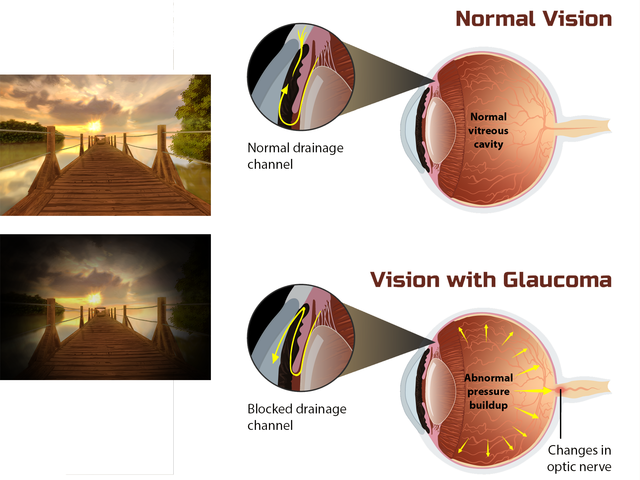
Primary open-angle glaucoma (POAG) is a chronic eye disease that causes progressive damage to the optic nerve over time. This damage often results in a gradual loss of vision, which can ultimately lead to blindness if left untreated. Unlike other types of glaucoma, OAG typically develops without noticeable symptoms at first, which is why it’s often called the “silent thief of sight.”
Understanding Primary Open-Angle Glaucoma
Primary open-angle glaucoma is the most common type, accounting for over 70% of all glaucoma cases. POAG prevalence varies globally, but it is suggested that 57.5 million individuals have the disease worldwide. The disease’s prevalence increases with age, with individuals over 60 at the highest risk. Also, those with severe OAG are at an increased risk of falls or fractures due to impaired vision and decreased mobility.
The most common signs and symptoms of POAG are changes in peripheral vision, eye redness, eye pain, halos around lights, blurred vision, and tunnel vision. However, these symptoms often occur late in the disease course, indicating the risk of severe vision loss.
The disease usually results from inadequate drainage of the aqueous humor through the trabecular meshwork, which leads to increased eye pressure. Unfortunately, the impacts of POAG on daily life can be challenging, as vision loss can lead to difficulties in driving, reading, and performing daily tasks.
Furthermore, individuals diagnosed with severe disease and disease progression face the most significant burden regarding eye-related expenses. This includes costs associated with treatments, medications, and frequent doctor visits.
Effective therapies that can slow down the advancement of the disease are crucial to bring about significant clinical benefits, preserving vision, and alleviating the substantial economic burden faced by patients and healthcare systems alike. While medical therapy is often the initial approach for managing glaucoma, patient adherence to medication can be suboptimal; thus, minimally invasive glaucoma surgery (MIGS) has been developed as a new treatment option.
More on Minimally Invasive Glaucoma Surgery
Compared to traditional incisional surgery, MIGS is less invasive and has a shorter recovery time. They also have a lower risk of complications, such as bleeding or infection, and may not require general anesthesia. These procedures typically involve using canal-based or suprachoroidal-based devices inserted into the eye to reduce intraocular pressure.
Canal-based devices increase the drainage of aqueous humor, the fluid that fills the front of the eye. On the other hand, suprachoroidal-based devices work by shunting fluid from the front of the eye to the space between the sclera and the choroid, a layer of blood vessels in the eye.
It is worth noting that MIGS devices that form a bleb have been associated with substantial intraocular pressure reductions. A bleb is a fluid-filled pocket that forms under the conjunctiva, the thin membrane covering the eye’s white part. The formation and management of the bleb play a critical role in surgical success. Surgeons can effectively regulate intraocular pressure and improve patient outcomes by carefully managing the bleb.
What are Microshunts?
Researchers have developed a minimally invasive glaucoma surgery device known as the MicroShunt, which has shown promising results in reducing intraocular pressure and the usage of glaucoma medication.
The MicroShunt procedure involves creating a small incision on the eye’s surface. Then, the device is placed under the conjunctiva, the white part of the eye, and connected to the anterior chamber, which is the space between the iris and the cornea. The device allows excess fluid in the eye to drain, which reduces intraocular pressure and prevents further damage to the optic nerve.
Studies conducted in the Dominican Republic have shown that the MicroShunt has a high success rate of 95% at year 3 in reducing pressure. However, it is essential to note that, like any surgical procedure, there are potential adverse events, such as the device touching the iris, temporary low intraocular pressure, shallow or flat anterior chamber, and temporary choroidal effusion.
Still, MIGS devices like the MicroShunt offer a promising option for POAG patients as they are less invasive and effective than traditional glaucoma surgeries. While there are potential risks and complications associated with any surgical procedure, the MicroShunt has demonstrated effectiveness in reducing IOP and preserving vision. Early detection and treatment of POAG is crucial for the best possible outcomes, and MIGS devices like the MicroShunt provide an alternative treatment option for those with this condition.
To learn more about the eye, read more stories at www.williamhaseltine.com

