The Healing Code: Deciphering Vagus Nerve's Impact on Pediatric Gut Health
(Posted on Friday, November 17, 2023)
This article was originally published on Forbes on 11/17/23.
This story is part of a series on the current progression in Regenerative Medicine. This piece discusses advances in vagus nerve stimulation.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
A 2015 estimate from the CDC suggests that over three million adults suffer from Inflammatory Bowel Disease. Not included in this estimate are the hundreds of thousands of underage patients who also live with these chronic illnesses. Inflammatory Bowel Disease is the chronic inflammation of the gastrointestinal tract, most commonly in the form of Crohn’s disease or ulcerative colitis. While the exact cause is unknown, Inflammatory Bowel Disease typically results from weakened immune systems, which are often genetically inherited.
New noninvasive techniques may soon allow physicians to treat pediatric Inflammatory Bowel Disease without extensive surgical or prescription intervention. A recent study in Bioelectronic Medicine by Dr. Benjamin Sahn and colleagues from the Feinstein Institutes for Medical Research attenuated the effects of Inflammatory Bowel Disease in children using transcutaneous auricular vagus nerve stimulation. Here, I will discuss this technique and how it may be used in other forms of regenerative medicine.
The vagus nerve is among the most critical components of the nervous system, controlling several bodily functions, including digestion, heart rate, immune function, and more. Among these crucial functions is the anti-inflammation of the intestinal tract. Crohn’s disease and ulcerative colitis result from imbalances in the nervous system, specifically regarding the vagus nerve.
It has been reported in recent years that stimulation of the vagus nerve could be used to suppress inflammatory cytokines and reduce intestinal symptoms.
Sahn and colleagues aimed to replicate these results through a novel pathway. Their transcutaneous auricular vagus nerve stimulation is entirely noninvasive and delivered through an electrical device placed on the ear.
The ear is heavily intertwined via the nervous system to the vagus nerve, and different ear sections are interconnected with other vagus nerve functions. For our purposes, the flat area of the outer ear located towards the middle of the structure and above the ear canal, known as the cymba conchae, is closely associated with the vagus nerve’s digestive network.
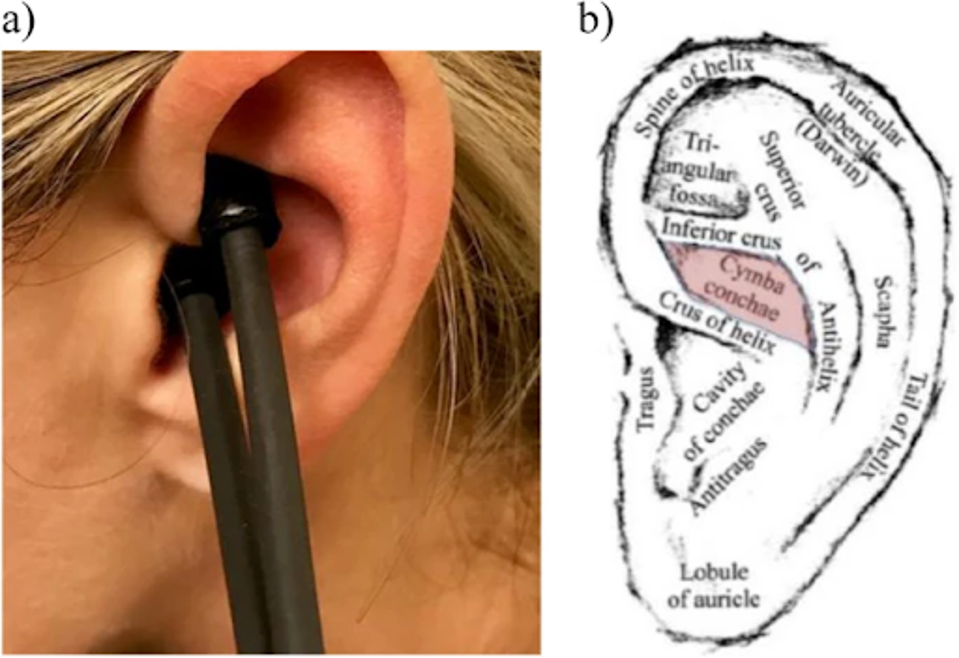
FIGURE 1: Transcutaneous Auricular Vagus Nerve Stimulation Method. (a) Hand-held sensor probe stimulating the cymba conchae area of the left ear. (b) Schematic of left ear with anatomic location of cymba conchae.
Using the sensor probe stimulation pictured above, Sahn and colleagues followed a cohort of 22 subjects ages 10-21 with mild to moderate Inflammatory Bowel Disease over 16 weeks. The first area of analysis was fecal calprotectin, a protein in the digestive tract that can be used as a biomarker for intestinal inflammation. The more fecal calprotectin in a stool sample, the greater the inflammation of the subject.
Over the first four-week period, the cohort was split into two subgroups, one receiving the treatment for the first two weeks and then receiving a placebo for the third and fourth weeks. The other subset was reversed, receiving treatment in the latter two weeks. They were instructed to use the stimulation once daily for five minutes.
Sahn and colleagues found that median fecal calprotectin increased by 308µg/g from the initial baseline during the placebo period. During the treatment period, the same metric decreased by 225µg/g, for a net difference of 533µg/g. This finding suggests that even with minimal use, transcutaneous auricular vagus nerve stimulation reduced overall bowel inflammation.
For weeks four through 16, the researchers increased the subject use of stimulation to twice daily, for five minutes per use in the morning and evening.
Using pediatric indexes to measure activity for Crohn’s disease and ulcerative colitis, the researchers found that most patients experienced a significant decrease in their symptoms while using vagus nerve stimulation. Some patients even achieved remission of their disease over the 16-week trial period.
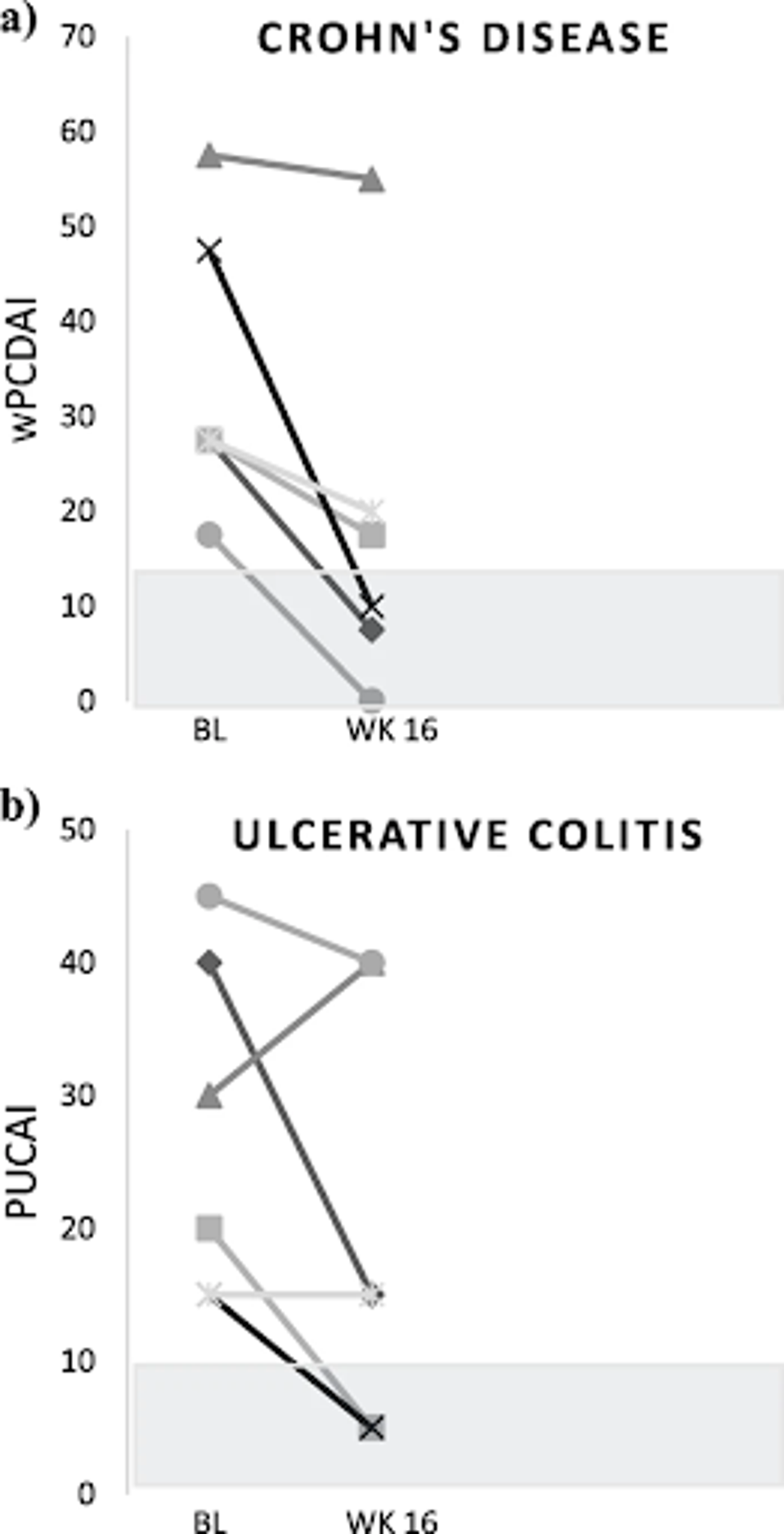
FIGURE 2: Change in IBD activity index from baseline (BL) to week (WK) 16. (a) wPCDAI = weighted pediatric Crohn’s disease activity index. (b) PUCAI = pediatric ulcerative colitis activity index. Shaded area represents remission zones.
Similar results were found with fecal calprotectin in the first four-week period. Over 82% of patients had a tangible decrease in fecal calprotectin detected, and over 64% had a greater than 50% decrease. Notably, reductions in fecal calprotectin were more pronounced in ulcerative colitis patients than those with Crohn’s disease.
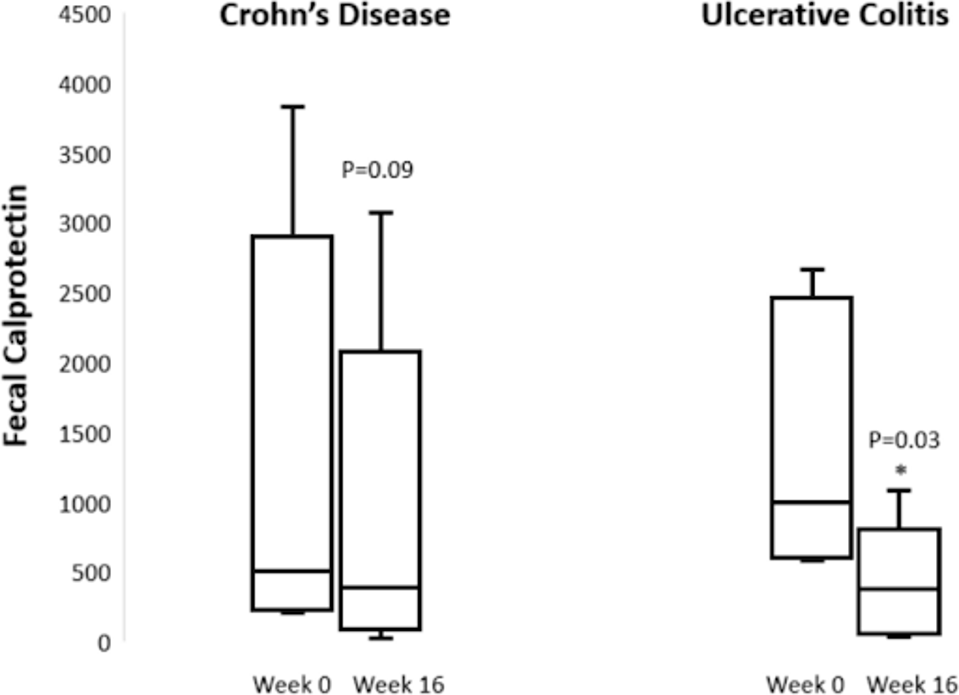
FIGURE 3: Change in Fecal Calprotectin by Diagnosis.
As with any medical intervention, there are always side effects to consider. With the vagus nerve so intimately involved in bodily functions, some effects are likely to occur. These include but are not limited to, throat pain, headache, shortness of breath, trouble swallowing and sleeping, the worsening of preexisting sleep apnea, and ear pain.
I have long written about the potential health therapies that could be brought about vagus nerve stimulation, whether that be reduction of inflammatory disease, or even assuaging Long Covid.
In addition to the therapeutic application of transcutaneous auricular vagus nerve stimulation for pediatric digestive disorders, there are also studies describing its use for speech therapy, treating depression, epilepsy, heart rate variability, or even pediatric neurodevelopment.
We have only scratched the surface of what the vagus nerve can impact. As Dr. Sahn and colleagues conducted here describing its benefit for Inflammatory Bowel Disease, I cannot wait to see how others use this emerging technology for therapeutic good in the near future.

