Advancing Pain Management: Exploring The Frontiers Of Electroanalgesia
(Posted on Friday, December 1, 2023)

This article was originally published on Forbes on 12/1/23.
This story is part of a series on the current progression in Regenerative Medicine. This piece discusses advances in electrotherapy.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
Chronic pain is among the most common ailments in the United States, affecting roughly 100 million adult Americans. Chronic pain, or persistent pain lasting three months or more, is both a primary condition as well as a common side effect of other chronic diseases. This mass pain fuels the ongoing opioid epidemic and plays a role in disability-related unemployment, poverty, and homelessness.
As such a significant hurdle in our healthcare system, all efforts should be made to investigate the possible avenues to treat chronic pain and curtail the epidemic.
In recent years, electroanalgesia, or electrotherapy, has arisen as a promising potential remedy. Dating back thousands of years to the Greco-Roman days of Aristotle and Plutarch, electroanalgensia involves precision electrical impulses targeted towards specific nerve endings involved in pain reception.
In a recent review for The New England Journal of Medicine, Dr. Thomas J Smith and colleagues from the Johns Hopkins School of Medicine investigated two forms of electroanalgensia: TENS therapy and scrambler therapy. Here, I will analyze their review and discuss the potential implications of these therapies.
Before discussing the intricacies of TENS and scrambler therapy, we must first understand the basics of cutaneous electroanalgesia, which is the use of electrical stimulation applied to the skin. When we feel pain, nerve receptors signal to the brain that something is wrong or damaged. These receptors, called nociceptors, are triggered by pressure, heat, and chemical stimuli, among other hazards. Chronic pain is the continuous overstimulation of nociceptors.
Cutaneous electroanalgesia applies electricity to the overloaded nociceptors in the skin to counteract the pain signals transmitted to the brain. The technique is completely noninvasive, meaning there are no needles, surgeries, or scarring, keeping the patient comfortable. Noninvasive techniques are also less expensive, ensuring electroanalgesia is more accessible to all experiencing chronic pain.
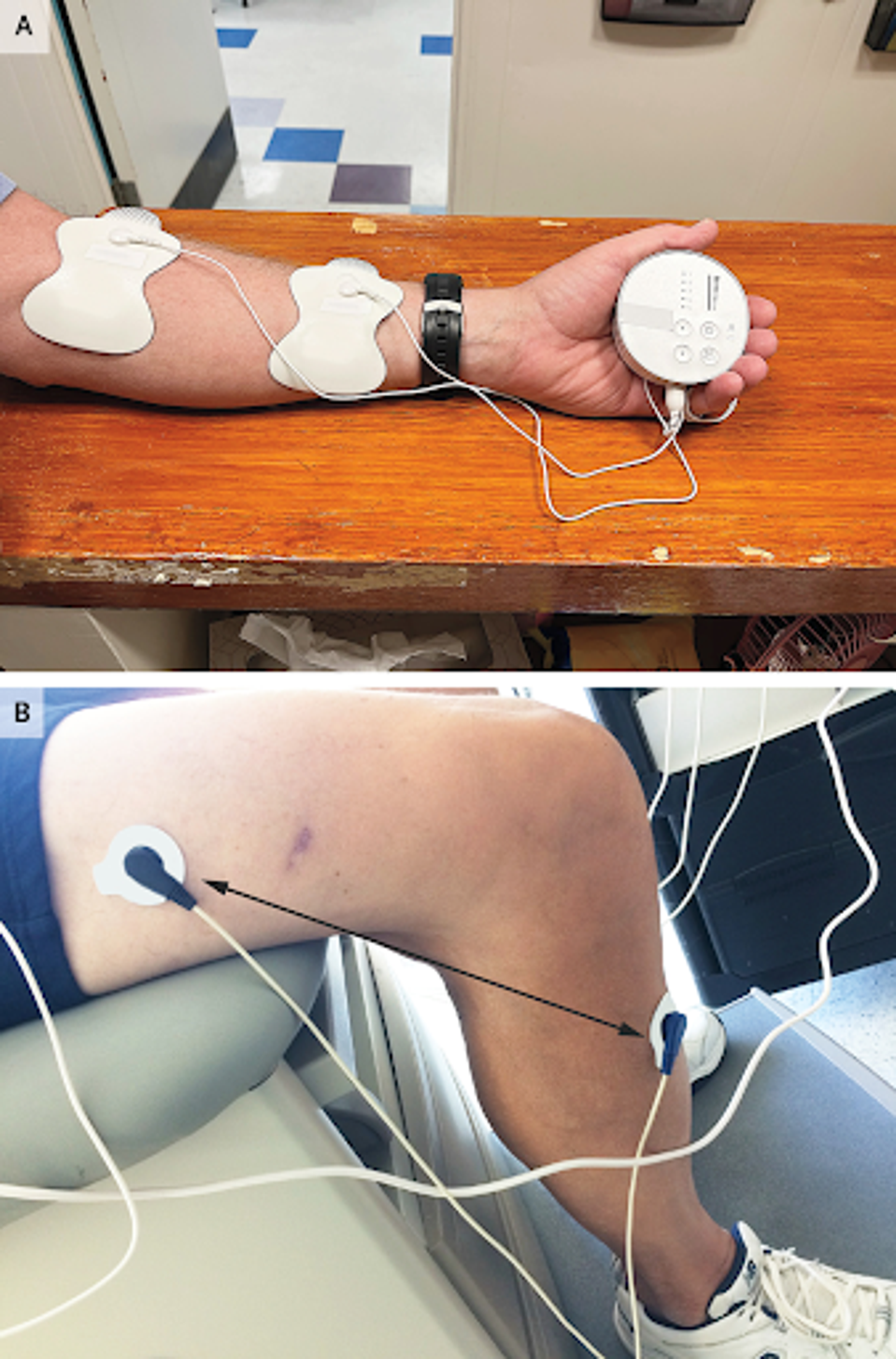
FIGURE 1: Application of TENS Electrodes and Use of Scrambler Therapy in a Patient with Chemotherapy-Induced Neuropathy.
Transcutaneous electrical nerve stimulation, or TENS, is a more traditional electroanalgesia treatment than scrambler therapy. It involves a TENS device that delivers electrical stimulation through targeted patches on the skin. The aim is to block the signals from leaving the nerve centers and making their way to the brain.
Scrambler therapy, on the other hand, takes a different approach. Rather than blocking signals from reaching the brain, a scrambler unit delivers electrical impulses that transmit artificial signals to the brain. These synthetic signals reach the same brain region that processes real pain signals, effectively scrambling the incoming data and reducing pain perception.
Scrambler therapy produces better outcomes than its TENS counterpart. Studies reviewed by Smith and colleagues show 80-90% effectiveness in reducing chronic pain symptoms over time with the scrambler system. The introduction of scrambler signals reduces pain during ongoing treatment cycles, and it has been documented that long-term pain reduction lasts months or even years after scrambler treatment. TENS, on the other hand, requires continuous treatment for continued pain relief.
However, TENS treatment is the more accessible of the two. The key advantage is that TENS treatment is typically self-administered and costs as low as $20, meaning anyone with access to the system can treat themselves whenever necessary. A scrambler device can cost upwards of $65,000 and must be administered by a professional, making the treatment much more expensive and less time-flexible.
Both treatments have the typical minimal side effects one would expect from an electrotherapy, including muscle soreness, fatigue, and skin irritation, but no moderate or severe reactions have been reported.
How, then, should we proceed with developing and implementing these treatments in the United States healthcare system?
As many as three million American citizens struggle with opioid addiction, most of which are impoverished. In my estimation, the TENS system is the immediate bandage that needs to be applied to the situation. While not as effective as the scrambler system, it is far more affordable and accessible to the people who need it most.
In the meantime, we should continue to develop the scrambler system and bring down the cost of the device to allow low and middle-income Americans access to its benefits. Ultimately, if the scrambler can be optimized to the point of affordability and self-administration found with the TENS system, the long-term benefits of relieving millions from chronic pain would be innumerable.

