Beyond Traditional Treatments: Laser Therapies for Diabetic Macular Edema
(Posted on Wednesday, January 3, 2024)
This story is part of a series on the current progression in Regenerative Medicine. This piece is part of a series dedicated to the eye and improvements in restoring vision.
In 1999, I defined regenerative medicine as the collection of interventions that restore tissues and organs damaged by disease, injured by trauma, or worn by time to normal function. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
Diabetic macular edema is a severe complication of diabetes that affects a person’s vision and can lead to blindness if left untreated. Diabetic macular edema (DME) is a leading cause of vision loss among people with diabetes, and its prevalence is increasing. More specifically, the University of Toronto found that the pooled prevalence of DME was approximately 5.5% among people with diabetes. However, the good news is that effective treatments are available, including laser photocoagulation therapy.
Laser therapy, specifically subthreshold and multimodal imaging-guided laser therapy techniques, has emerged as an essential treatment option for DME. These cutting-edge therapies are more precise, less invasive, and offer significant advantages over traditional laser therapy. They can reduce the need for frequent follow-up appointments, improve treatment outcomes, and significantly reduce patient treatment burden.
More on Diabetic Macular Edema
Diabetic macular edema (DME) is a severe complication of diabetes that can lead to vision loss and blindness if left untreated. It is a type of macular edema that occurs when fluid accumulates in the macula, which is the central part of the retina responsible for sharp, detailed vision.
DME is caused by damage to the retina’s blood vessels due to high blood sugar levels over time. This damage causes the blood vessels to leak fluid into the macula, leading to swelling and distortion of the central vision. Symptoms include blurred or distorted vision, difficulty reading or recognizing faces, and dark or empty spots in the central vision. If left untreated, it can cause permanent damage to the retina and lead to severe vision loss or blindness.
The condition is chronic and progressive, so early detection and prompt treatment are essential to prevent severe vision loss. Fortunately, effective treatments are available, including medications that can be injected into the eye to reduce swelling and improve vision.
The first-line treatment is anti-vascular endothelial growth factor (VEGF) therapy, which involves injections into the eye to prevent the growth of abnormal blood vessels that can contribute to edema. However, laser photocoagulation therapy can also be used as an alternative or in conjunction with anti-VEGF therapy.
What is Laser Photocoagulation?
Laser photocoagulation therapy involves using a laser to create thermal burns on the retina, which seal leaking blood vessels and reduce edema. The treatment has been used for DME for over 30 years and effectively reduces vision loss. Focal laser photocoagulation is the most commonly used technique, which targets microaneurysms or tiny fluid-filled sacs on the retina. The treatment is usually performed in an outpatient setting and can be completed in a single session.
Despite the effectiveness of laser photocoagulation therapy, its use has declined with the advent of anti-VEGF therapy. However, recent research by Nagoya City University has shown that laser therapy remains a practical therapeutic approach to chronic refractory edema. The key to successful laser therapy is identifying microaneurysms using multimodal, highly accurate, and minimally invasive coagulation techniques.
The image that is displayed below provides a comprehensive summary of the different types and settings of laser therapies that are currently available. In particular, the figure highlights two different types of laser therapy: focal and subthreshold.
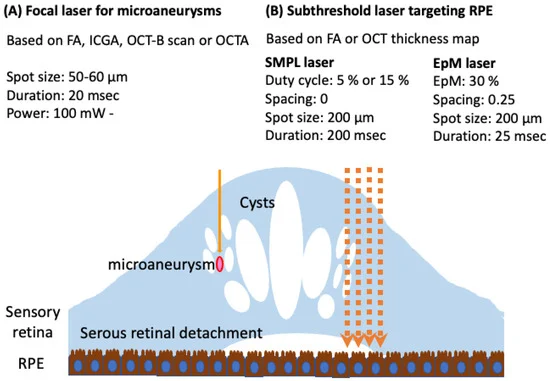
Focal laser therapy is used to target microaneurysms in the eye, and it is recommended that the duration of laser application should be kept short. The planning aspect of this therapy will involve the use of several imaging techniques such as fluorescein angiography (FA), indocyanine green angiography (ICGA), optical coherence tomography (OCT) B-scan, or OCT angiography (OCTA) to ensure accuracy.
Subthreshold laser therapy targets the retinal pigment epithelium (RPE). During the planning stage of this therapy, the image of the FA or OCT thickness map would be used to ensure the correct positioning of the laser.
Cutting-edge Laser Therapy Options
Furthermore, subthreshold laser therapy is a relatively new technique that uses lower energy levels than conventional laser therapy. This technique treats various retinal diseases, including diabetic macular edema and retinal vein occlusion. Subthreshold laser therapy has several advantages over traditional laser therapy.
Firstly, it reduces the frequency of anti-VEGF injections, often required in conjunction with laser therapy. This reduces the treatment burden on patients and improves their quality of life. Secondly, subthreshold laser therapy has the potential to provide longer-lasting treatment, which reduces the need for frequent follow-up appointments.
Multimodal imaging-guided laser therapy is another promising technique that combines various imaging modalities, such as optical coherence tomography (OCT), fundus photography, and fluorescein angiography. This technique allows for better visualization of microaneurysms, small bulges in the retina’s blood vessels that can cause vision loss.
Visualizing these microaneurysms makes it easier to target them with laser therapy. This technique can optimize anti-VEGF therapy and reduce treatment burden. Additionally, multimodal imaging-guided laser therapy can treat other retinal diseases, such as age-related macular degeneration and retinal vein occlusion.
Looking Forward
While anti-VEGF therapy remains the first-line treatment, laser therapy can be used as an alternative or in combination with anti-VEGF therapy. Using precise, minimally invasive coagulation techniques, such as multimodal imaging-guided and subthreshold laser therapy, can improve treatment outcomes and reduce treatment burden.
Further studies are needed to determine the optimal timing and settings for laser photocoagulation therapy and the potential of new laser technologies in managing DME. Nevertheless, laser photocoagulation therapy remains a valuable treatment option for DME, and its use should be considered in the management of this chronic and progressive condition.
To learn more about the eye, read more stories at www.williamhaseltine.com

