Using Responsive Deep Brain Stimulation for OCD
(Posted on Friday, January 12, 2024)

This article was originally published on Forbes on 1/12/24.
This story is part of a series on the current progression in Regenerative Medicine. This piece discusses advances in brain stimulation therapies.
In 1999, I defined regenerative medicine as the collection of interventions that restore normal function to tissues and organs damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
An emerging brain stimulation method could be the next great asset to treating obsessive-compulsive disorder in over two million adults in the United States. In Cell, Dr. Young-Hoon Nho and colleagues from the University of Pennsylvania and elsewhere report the first-in-human application of responsive deep brain stimulation for obsessive-compulsive disorder. Their results showed rapid and robust improvement in patient mental health symptoms, paving the way for a new personalized therapy in the near future.
Obsessive-compulsive disorder is a mental health disorder characterized by a series of obsessions in the form of recurring, unwanted thoughts, ideas, or sensations and compulsions, namely repetitive, difficult-to-control behaviors. Obsessions will cause the patient intense anxiety or distress, while compulsions will elicit those emotions if the compulsion is not performed.
Obsessive-compulsive disorder is thought to be caused by some combination of genetic, neurobiological, and environmental factors, often in a patient’s youth. While there is no cure, cognitive-behavior therapy and selective serotonin reuptake inhibitors are common pathways for symptom reduction.
Dr. Nho and colleagues approach obsessive-compulsive disorder treatment from a different perspective. Rather than maximizing symptom reduction, the researchers aimed to treat the disorder at the source, more akin to a cure.
In previous brain scans of patients suffering from the disorder, there are documented neural activity spikes in the ventral striatal regions of the brain, likely induced by stress related to a patient’s obsessions and compulsions.
Nho and colleagues theorized that targeted brain stimulation to these regions could alleviate the intensity of the obsessions and compulsions felt by the patients, leading to relieved anxiety, stress, headache, and other symptoms.
Deep brain stimulation is the implantation of electrodes in selective brain regions. These electrodes deliver low amperage impulses to modulate neural activity, in this case, in the ventral striatal region.
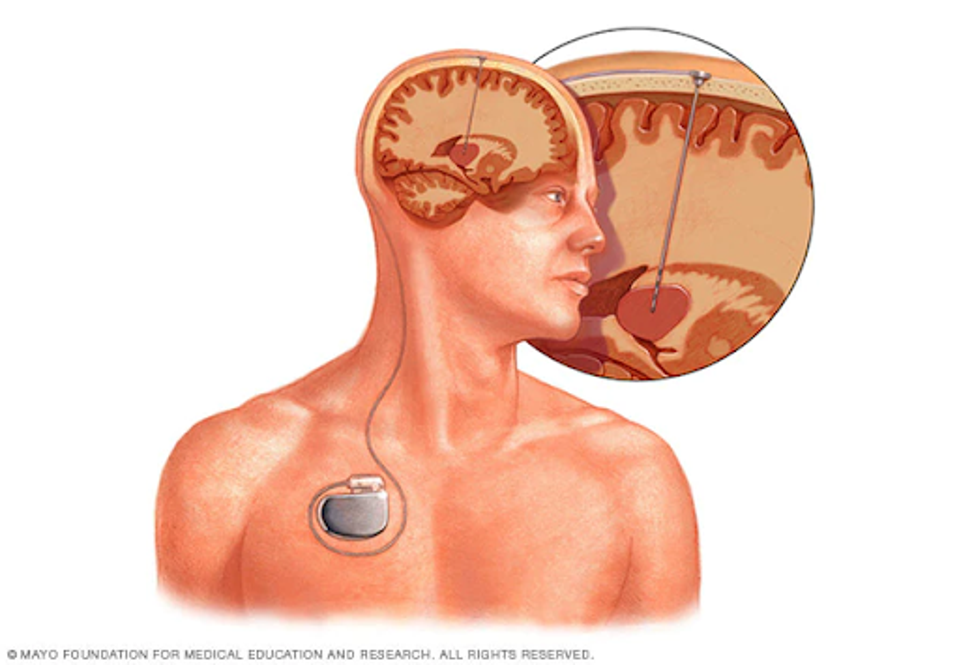
FIGURE 1: Schematic representation of a deep brain stimulation device.
Nho and colleagues did not initially use deep brain stimulation in humans for the treatment of obsessive-compulsive disorder. Instead, they implanted two electrodes in a patient suffering from seizures, who also was previously diagnosed with the disorder. The electrode leads were embedded in a similar brain region to that which experiences neural activity due to obsessive-compulsive disorder.
To create a baseline, they monitored both the patient’s neural activity in the targeted region and that of a control patient without the disorder during various tasks, such as reading or accomplishing a task in virtual reality.
The researchers monitored the patient for over two years, using the brain stimulation device regularly. The patient’s disorder-related symptoms reduced dramatically on both objective and subjective accounts.
Using the Yale-Brown Obsessive-Compulsive Scale, the patient’s obsessive-compulsive score reduced from 32 to 20 pre- and post-implant, a 37.5% reduction from baseline. Over time, that score decreased to 8 two years after implantation, a total reduction of 75%.
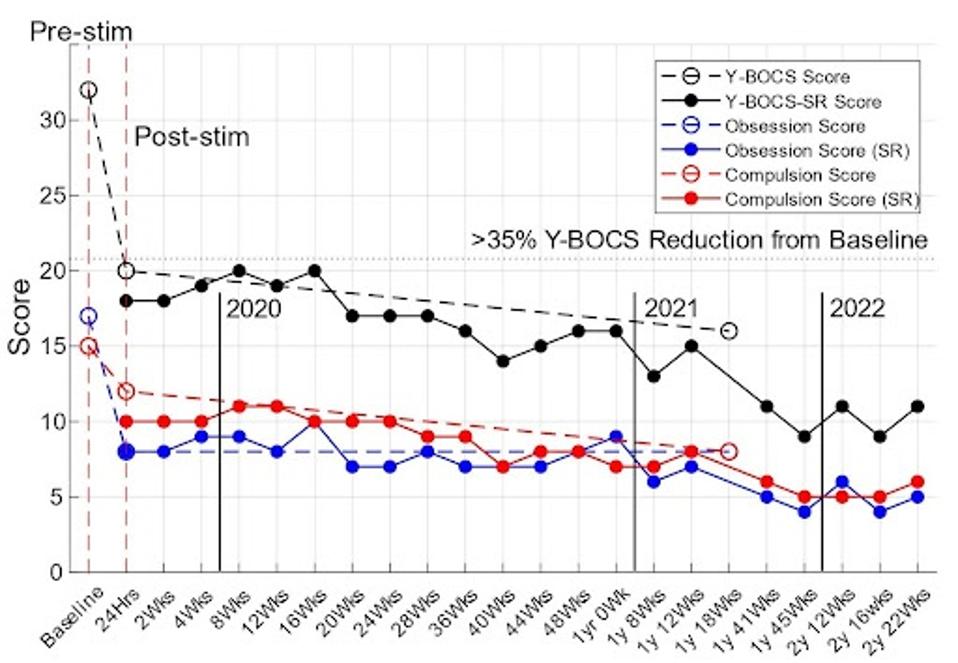
FIGURE 2: rDBS therapeutic outcomes
Furthermore, when discussing the stimulation outcomes with the patient, they described they were “no longer experiencing some of her obsessions and, consequently, was not feeling the urge to engage in compulsive behaviors, including several of her safety-related checking routines” and concluded by saying “she has had a life-changing improvement in her OCD symptoms.”
While it is hard to dispute the objective and subjective outcomes described by doctors and patients, there are some caveats to the results.
First, there was only one patient in the tested cohort, meaning more extensive human trials would be necessary before deep brain stimulation could move to the larger public.
Second, it is unclear whether the reduced activity in the ventral striatal region reduced symptom severity or if the stimulation impacted some other brain function, reducing obsessions and compulsions, resulting in reduced activity. Further testing on this method is the next step.
However, brain stimulation has long been a commonly used treatment for a range of neural conditions, such as Parkinson’s, epilepsy, Tourette’s, and depression, to name a few. While there may be some side effects, such as headache, nausea, or even stroke in rare cases, the practice could reduce dependence on medication and has the potential for long-term health benefits. I look forward to seeing its advancing use in the years to come to treat a swathe of debilitating neural disorders.

