How Do We Remember? Association Is The Key
(Posted on Wednesday, March 6, 2024)

This article was originally published on Forbes on 3/6/24.
This story is part of a series on the current progression in Regenerative Medicine. This piece discusses advances in neuroscience.
In 1999, I defined regenerative medicine as the collection of interventions that restore normal function to tissues and organs damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
A recent study has found a clue pointing to how we develop associative memories. This could be greatly beneficial to those struggling with memory-damaging diseases, such as Alzheimer’s. Here, we will analyze their findings and suggest how this may be used in a regenerative medicine context in the near future.
Most of our memories are non-associative. We recall a memory of a specific object, whether a person, place, or thing, and we picture that object to some degree of detail in our mind.
Associative memory is a level deeper. When a specific smell triggers a memory of the time you went on a trip as a child or hearing a name reminds you of a time you spent with a particular person, these are associative memories—connections between two ideas brought together by our subjective experience.
How are these complex connections made? For decades, we have known that the brain’s memory center is the hippocampus, but the mechanisms behind associative memory remained largely unresearched.
Dr. Lukas Kunz and colleagues from the University of Freiburg in Germany released a recent study in Nature that found that specific neurons in the medial temporal lobe were highly coactive with human associative memory.
In other words, when we establish an associative memory between two distinct objects, we learn that memory through repeated interaction. We cannot remember the face of the person we sat across from on the train because that was not enough of a stimulus. Neurons in the medial temporal lobe activate to process seeing that person’s face, but the memory is not ingrained in the hippocampus.
However, if you see this person every day for several weeks or months, those neurons are regularly stimulated with the same data, creating a memory. Associatively, when you recall sitting on the train, you may also see that person’s face or vice versa.
When an associative memory is recalled, the neuronal activity initially stimulated during the creation of the memory is reactivated alongside a hippocampal ripple. This oscillatory brain wave pattern triggers during moments of recollection, often during sleep.
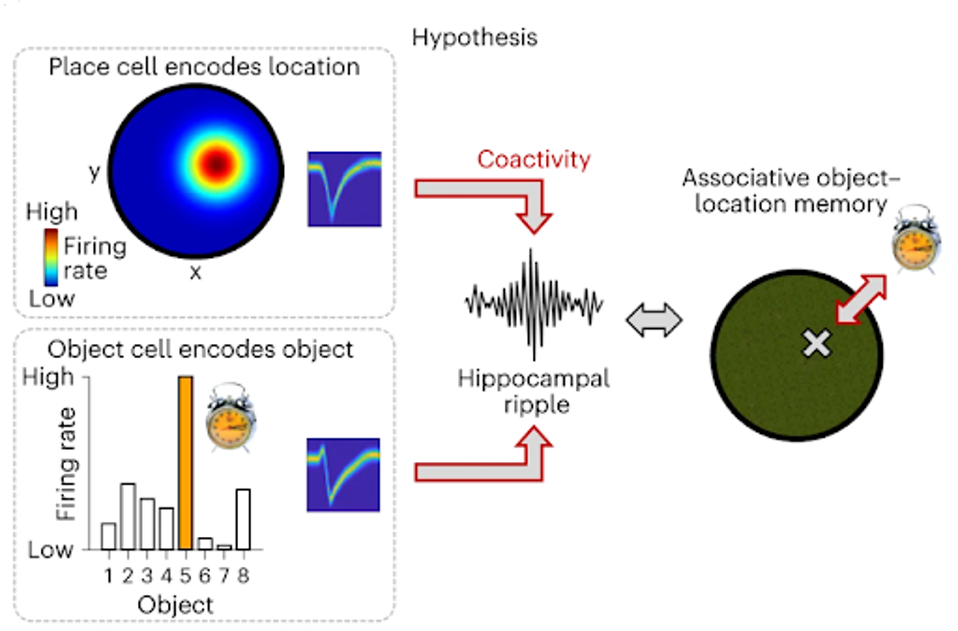
FIGURE 1: Human associative object–location memory is linked to the coactivity of object cells and place cells during hippocampal ripples.
Dr. Kunz and colleagues uncovered this coactivation by monitoring subjects as they participated in memory tasks. Participants encoded the locations of eight objects in a virtual environment and were tasked with remembering the object and its location. The researchers noted significant localized activity in the medial temporal lobe during both initial encoding periods.
Later, when the participants were tasked with recollecting the objects and their locations, the same neurons in the medial temporal lobe were firing alongside brain wave hippocampal ripples.
Further, the researchers noted that as participants repeated recollection periods, their memory performance improved alongside neuron and ripple activity fluctuations, suggesting an ever-evolving state of neural activity depending on familiarity with a given memory.
Regarding regenerative medicine, this research could take us in many different directions. First and foremost, this research could lead to a better understanding of neurodegenerative disease and injury that leads to memory loss. Age-associated memory impairment affects roughly 40% of elderly Americans, many of whom will progress to diseases such as Alzheimer’s. With targetted neuron stimulation, perhaps some memory loss could be prevented or even reversed.
Secondly, from a brain-machine interface perspective, this research could lead to the development of more advanced neuroprosthetics, potentially offering therapeutic benefits to individuals with memory impairments.
Thirdly, and perhaps the most science fiction adjacent to the three, we could see artificial memory development or alteration of memory. If an individual wanted to forget a troublesome memory, they could be free of the burden, or if someone wanted to experience something new, they could virtually relive an artificial memory. Once thought impossible, these ideas are more and more feasible by the day.
I highly anticipate further research in this field, as it could significantly impact regenerative medicine and the human experience as we know it.

