Forty years of HIV research inspires the development of SARS-CoV-2 therapy
(Posted on Monday, July 1, 2024)
Originally published October 23, 2023.
Almost four decades ago, the characterization of the human immunodeficiency virus type 1 (HIV-1) genome with the participation of the Haseltine laboratory at Harvard Medical School (Ratner et al., 1985) ushered in the antiretroviral era and established the framework for the genomic- and later multiple omics-based development of targeted antiviral drugs. Battles with pandemic HIV-1 taught us that multitargeted combination antiviral therapy is needed to control pathogens that rapidly adapt to selective pressures from the immune system, vaccines, and therapeutic monoclonal antibodies, such as pandemic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) strains. The development of therapeutics active against all SARS-CoV-2 variants of concern and human coronaviruses could be expedited by taking approaches used for developing the inhibitors of HIV-1 integrase and capsid as well as hepatitis C virus, such as rationale-based drug design aided by generative artificial intelligence and chemistry. Here, we provide examples of cross-pollination between researches on HIV-1 and SARS-CoV-2 to identify potential SARS-CoV-2 therapeutic targets at various lifecycle stages.
SARS-CoV-2 variants isolated by early 2020 showed a midrange annual substitution rate of 3 × 10−4 per site. Almost half were C→U transitions, with the highest proportions in the proximal and distal untranslated regions. Similarly, human APOBEC3 proteins induce C→U transitions in the HIV-1 genome, resulting in antiviral RNA editing and drug resistance (Ratcliff and Simmonds, 2023). Since late 2020, SARS-CoV-2 has exhibited major changes with substantially altered transmissibility and immune escape through the consecutive, independent, and dominant emergence of variants of concern. In response to the increased pressure from imprinted SARS-CoV-2 humoral immunity (Cao et al., 2023), mutations are driven predominantly by convergent evolution in the spike and accessory proteins of Omicron to aid in transmissibility, immune evasion, tropism shift, and viral entry into the cell. Similarly, convergent evolution at specific hotspots is observed during the evolution of HIV-1 (Fantini et al., 2023). One valuable takeaway from HIV-1 research, where an effective vaccine or cure is still lacking, is that the combination therapy could effectively suppress the virus while reducing the risk of resistance development. Combination therapies, possibly along with pan-coronavirus vaccines that are more durable and less affected by viral variation than the currently available ones for SARS-CoV-2, are needed to prepare for pandemics of SARS-CoV-2 and other human coronaviruses. The established research and manufacturing infrastructures, as well as programs for universal access to medications and healthcare, can then contribute to readiness for all pathogens.
Among the examples listed in Table 1, the nirmatrelvir–ritonavir combination illustrates the accelerated generation of an antiviral against SARS-CoV-2. Although known HIV-1 protease inhibitors do not significantly inhibit the main protease nonstructural protein 5 (NSP5) of SARS‐CoV‐2 in vitro, lopinavir can inhibit the protease of SARS‐CoV‐1. This finding, combined with real-world evidence that an inhibitor of the main coronaviral protease effectively treats feline infectious peritonitis, inspired the development of nirmatrelvir. Oral nirmatrelvir, boosted with ritonavir to inhibit its cytochrome P450 3A4-mediated metabolism, similar to lopinavir action in treating HIV-1 infection, was approved for the treatment of mild-to-moderate coronavirus disease 2019 (COVID-19) within five days of SARS-CoV-2 infection diagnosis. However, rebound viremia, which in some cases may reflect reinfection, has been observed after treatment with nirmatrelvir–ritonavir.
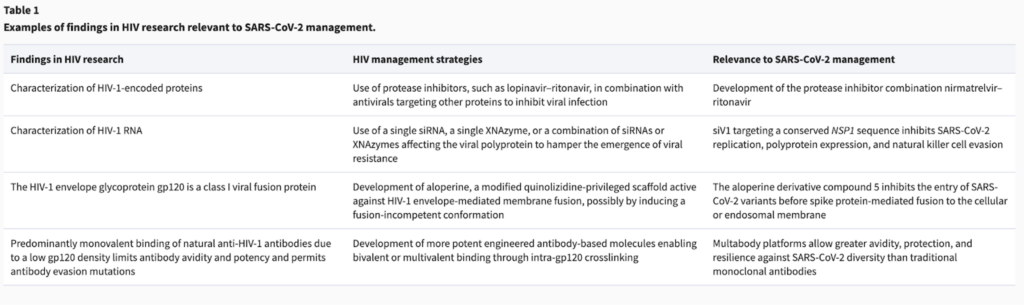
The need for combination antiviral therapy has also been illustrated with nucleic acid-based therapies. For HIV-1, the use of single small interfering RNAs (siRNAs), i.e. double-stranded RNAs that protect cells by degrading exogenous messenger RNAs (mRNAs), leads to the emergence of viral resistance, while combinations of siRNAs hamper this consequence. For SARS-CoV-2, siV1 has been identified to efficiently target NSP1 RNA. siV1 almost completely inhibits SARS-CoV-2 replication in cell culture without toxicity or induction of type I/III interferon production, and its target sequence is highly conserved in SARS-CoV-2 variants (Friedrich et al., 2022). Because NSP1 is part of a polyprotein that includes other SARS-CoV-2 NSPs such as NSP5, the inhibition of NSP1 expression could also affect SARS-CoV-2 polyprotein expression and immune evasion. HIV-1 downregulates the expression of natural killer cell activating receptors in host cells as part of innate immunity. Likewise, via NSP1 action,
SARS-CoV-2 shields infected cells from recognition and killing by natural killer cells (Lee et al., 2022; Table 1).
XNAzymes are modular nucleic acid catalysts capable of sequence-specific RNA transesterification and target mRNA cleavage with high specificity. Targeting multiple RNA sequences using a multifunctional construct or cocktail of XNAzymes reduces the emergence of escape variants compared with targeting a single site of rapidly mutating RNA viruses such as HIV-1. This is particularly relevant to proteins encoded by different open reading frames, such as the SARS-CoV-2 spike protein, rather than the large proximal polyproteins. A combined XNAzyme strategy may prevent virus from blocking the silencing machinery in host cells and reduce the disruption of host regulatory networks. This approach may also enable RNA knockdown in subcellular compartments or extracellular vesicles, where host effectors, such as replication organelles or exosomes involved in the cell-to-cell transfer of viral components, are scarce or unavailable, as observed for SARS-CoV-2 (Barberis et al., 2021; Table 1).
Both HIV-1 and SARS-CoV-2 are lipid-enveloped viruses. The HIV-1 envelope glycoprotein gp120 and the SARS-CoV-2 spike protein are class I viral fusion proteins. After binding to their main cognate cellular receptors, cluster of differentiation 4 (CD4) for HIV-1 and angiotensin converting enzyme 2 (ACE2) for SARS-CoV-2, both proteins require priming by cell surface proteases to mediate host cell entry, the first step in the viral lifecycle and a potential antiviral target. Aloperine is a quinolizidine-privileged scaffold modified to be a specific antiviral with improved potency against HIV-1 envelope-mediated membrane fusion, possibly by inducing a fusion-incompetent conformation. The aloperine derivative compound 5 most potently inhibits the entry of SARS-CoV-2 variants D614G, Delta, and Omicron before they fuse to the cell or endosomal membrane (Huang et al., 2022; Table 1).
The methyltransferase phosphorylated C-terminal domain-interacting factor 1 (PCIF1) inhibits HIV-1 infection by stabilizing the ETS1 proto-oncogene transcription factor that binds to the HIV-1 promoter to regulate viral transcription; as a countermeasure, the HIV-1 viral protein R interacts with PCIF1 and induces PCIF1 ubiquitination and degradation. For SARS-CoV-2 and other coronaviruses, PCIF1 promotes infection by sustaining the expression of its cognate ACE2 receptor and the cell surface protease TMPRSS2 via N6,2′-O-dimethyladenosine-dependent mRNA stabilization, a modification proximal to the 7-methylguanosine cap structure (Wang et al., 2023a).
Demethylation by lysine-specific demethylase 1 (LSD1) is required for the activation of HIV-1 transcription by its tat protein. For SARS-CoV-2 infection, LSD1 couples with ACE2 to enhance the cell surface ACE2–viral spike interaction during viral entry. LSD1 also favors the interaction between ACE2 and the nuclear import protein importin-α to increase the level of nuclear RNA polymerase II-coupled ACE2. This led to the development of a novel, durable, and cell-permeable nuclear ACE2 inhibitor, which significantly inhibits SARS-CoV-2 cellular replication for post-exposure prophylaxis without abolishing the cell surface ACE2 needed for cellular immunoprotection (Tu et al., 2023).
HIV-1 and SARS-CoV-2 interact with multiple receptors (such as CD147 for both viruses) and co-receptors (Pak et al., 2022), which are potential therapeutic targets because multivalent binding optimizes viral residence time and affinity to the host cell membrane. Multivalent binding is also important for improving therapeutics. For instance, anti-HIV-1 antibodies primarily bind monovalently because the low density of HIV-1 gp120 impedes bivalent binding through inter-gp120 crosslinking. Monovalent binding reduces avidity and potency, thus expanding the range of mutations permitting antibody evasion. In contrast, engineered antibody-based molecules are able to bind bivalently and their potencies increase by up to 2.5 orders of magnitude. Likewise, among natural immunoglobulin G (IgG) targeting the receptor-binding domain-2 epitope on SARS-CoV-2, nearly all Omicron neutralizers recognize both antigen-binding fragments and adjacent receptor-binding domains on the same trimeric spike, while the others that do not neutralize Omicron exhibit entirely or 22%–50% monovalent occupancy. Therefore, vaccine strategies targeting future SARS-CoV-2 variants should consider the epitope display with spacing and organization identical to trimeric spikes (Callaway et al., 2023). Moreover, multi-specific and multi-affinity antibody (Multabody) platforms have been developed for HIV-1 and later for SARS-CoV-2. A Multabody derived from the human apoferritin promoter enables multimerization of antibody fragments targeting three regions within the SARS-CoV-2 receptor-binding domain, which is the target of most clinical antibodies against SARS-CoV-2. The Multabody is more potent on neurilizing SARS-CoV-2 in mice (at a 30-fold lower dose) than a cocktail of the corresponding individual monoclonal antibodies. Additionally, mono-specific Multabodies potently neutralize SARS-CoV-2 variants of concern because of their augmented avidity, and tri-specific Multabodies expand the neutralization breadth beyond SARS-CoV-2 to other sarbecoviruses. Therefore, combining avidity and multi-specificity can confer protection and resilience against viral diversity, exceeding those provided by traditional monoclonal antibody therapies (Burn Aschner et al., 2023; Table 1).
The surface proteins of HIV-1 and SARS-CoV-2 are highly glycosylated, and both viruses rely on the expression of specific oligosaccharides to evade detection by the host immune system. HIV-1 gp120 contains more glycans than amino acids. Thus, glycan trimming is implemented in single-component, self-assembling protein nanoparticles, which display native-like HIV-1 envelope trimers, as vaccine candidates. This vaccine strategy could improve recognition of the CD4 binding site, without impacting the broadly neutralizing antibodies that target major glycan epitopes, and also increase the frequency of vaccine responders in various animal models (Zhang et al., 2023). For SARS-CoV-2, 15 out of 22 N-linked glycan attachment sites on its spike protein are shared among 12 sarbecoviruses. Their glycan attachment sites in the C-terminal S2 domain are highly conserved with a low abundance of oligomannose-type glycans, i.e. a low glycan shield density, which may provide a target to generate a pan-coronavirus antibody response (Allen et al., 2023).
SARS-CoV-2 has a large, complex, linear, non-segmented, polycistronic, positive-sense, and single-stranded RNA genome. Following both continuous and discontinuous replication strategies, RNA-dependent RNA polymerase uses the genome as a template to generate negative-sense subgenome- and genome-length RNAs, which are in turn used as templates for the synthesis of positive-sense full-length progeny genomes and subgenomic RNAs. The transcriptome of SARS-CoV-2 might also include protein-encoding RNAs that are transcribed from negative-sense genomic RNA, as documented for the transcriptomes of retroviruses. For instance, HIV-1 encodes the antisense protein, which is likely a structural protein to associate with gp120 and functionally involved in autophagy regulation, and human T-cell leukemia virus type 1 (HTLV-1) encodes the bZIP factor involved in oncogenesis (Lin et al., 2022). Beside coding for proteins in the cytoplasm, mRNAs of retroviral antisense genes localize to the nucleus of infected cells via inefficient polyadenylation induced by the 3′ long terminal repeat and regulate transcription directly by acting as long noncoding RNAs. For example, HTLV-1 antisense mRNA interacts with the promoter and enhances the transcription of the C–C chemokine receptor type 4 gene to support the proliferation of HTLV-1-infected cells, and HIV-1 antisense mRNA is recruited to the viral long terminal repeat and inhibits sense mRNA expression to maintain the latency of HIV-1 infection (Li et al., 2023). The antiviral remdesivir is a nucleotide prodrug of an adenosine analog, which binds to RNA-dependent RNA polymerase and inhibits viral replication by terminating RNA transcription prematurely.
As the final feature shared by HIV-1 and SARS-CoV-2, infection by either virus might accelerate human aging and human cellular senescence (Teulière et al., 2023). Optimizing immune resilience may preserve and/or rapidly restore immune functions that promote disease resistance (immunocompetence) and control inflammation caused by infec-tious diseases or other inflammatory stresses. This concept is assessed using peripheral blood metrics, including the balance between CD8+ and CD4+ T-cell levels and gene expression signatures that track longevity-associated immuno-competence and mortality-associated inflammation. The preservation of optimal immune resilience reduces the risk of HIV acquisition, acquired immune deficiency syndrome development, symptomatic influenza infection, and recurrent skin cancer, improves the survival rate during COVID-19 and sepsis, and increases longevity (Ahuja et al., 2023). To this end, understanding the viral impacts on host chromatin and epigenome will not only provide new strategies to fight SARS-CoV-2 and HIV-1 in the acute phase but also pave the way for unraveling the molecular basis of their long-term sequelae for intervention (Wang et al., 2023b).
Read the original manuscript in the Journal of Molecular Cell Biology.

