Patti Scialfa's Cancer Diagnosis: What To Know About Multiple Myeloma
(Posted on Wednesday, September 18, 2024)

NEW YORK, NY – JUNE 10: Bruce Springsteen and Patti Scialfa attend the 72nd Annual Tony Awards at Radio City Music Hall on June 10, 2018 in New York City. (Photo by Jemal Countess/Getty Images for Tony Awards Productions )
Getty Images for Tony Awards Productions
Patti Scialfa, Bruce Springsteen’s wife and bandmate, recently revealed she was diagnosed in 2018 with a rare blood cancer called multiple myeloma.
The 71-year-old has sung and strummed alongside Bruce Springsteen as a backup vocalist and guitarist for over four decades. Since joining the E Street Band in 1984, Scialfa helped create hits like “Dancing in the Dark” and “Born in the U.S.A.,” which shaped music of that era and earned the group a place in the 2014 Rock & Roll Hall of Fame. Though the E Street band is still active today, these days Scialfa is notably absent from the lineup.
Scialfa has pulled back from touring since her myeloma diagnosis. She shares her story in the documentary Road Diary: Bruce Springsteen and the E Street Band, which premiered at the Toronto Film Festival. Multiple myeloma “affects my immune system, so I have to be careful what I choose to do and where I choose to go,” she explains in the film. “Every once in a while, I come to a show or two and I can sing a few songs on stage, and that’s been a treat. That’s the new normal for me right now, and I’m OK with that.”
What Is Multiple Myeloma?
Patti Scialfa’s cancer diagnosis has taken her off the stage and imposed new limits on her body. But what exactly is multiple myeloma, and how does it impact one’s life?
Multiple myeloma is a blood cancer that impacts plasma B cells, a type of white blood cell found in the bone marrow. Plasma cells usually protect the immune system by producing antibodies. However, for people with myeloma, these plasma cells no longer keep the body safe; they produce abnormal, damaging antibodies and multiply faster than the body can handle. They crowd out healthy red blood cells and harm multiple bones throughout the body, including the spine, pelvis and ribs—thus the name “multiple” myeloma. The cancer cells can also spread beyond the bone marrow to other organs.
Just as Scialfa states in the documentary, multiple myeloma affects the immune system. It may not be noticeable at first since most people are initially asymptomatic. As the cancer increasingly sets the body off-balance, a wide range of symptoms can emerge:
- Frequent infections
- Bone pains in the back, ribs and hips
- Fatigue caused by anemia (low red blood cell count)
- Weakness in the limbs
- Extreme thirst and confusion
- Headaches, weight loss, bruising and more
Most people only discover they have myeloma after symptoms have persisted for some time or after routine blood tests.
More than 35,000 people in the U.S. will be diagnosed with multiple myeloma this year. It’s rare — less than 1% of men and women will develop this illness at some point in their life — but certain risk factors increase this likelihood, such as excess weight, African American descent, a family history of multiple myeloma and older age, with the average age of diagnosis at around 65 years old.

NEW YORK – OCTOBER 13: Patti Scialfa is joined on stage by her husband Bruce Springsteen during the Vote For Change concert at the Continental Airlines Arena October 13, 2004 in East Rutherford, New Jersey. (Photo by Paul Hawthorne/Getty Images)
Getty Images
How Do You Treat Multiple Myeloma?
What treatments would someone like Scialfa undergo to treat their myeloma?
Options vary depending on how severe the disease is and if they are eligible for an autologous stem cell transplant. A transplant can benefit patients significantly by renewing the bone marrow’s ability to produce healthy blood cells. For this procedure, a patient’s blood stem cells are taken and stored until after treatment to kill cancer cells. Then, the cells are infused back into the bloodstream through an IV.
Most patients — transplant candidates or not — begin a triple-drug combination treatment that includes:
- Oral medications known as immunomodulators. These drugs stimulate the immune system to fight cancer.
- Injections that block a protein complex called proteasomes in cells. When this complex is blocked in cancer cells, proteins build up inside and cause the cell’s death
- Steroids that help the other drugs work better and kill myeloma cells.
After patients undergo several rounds of this regime, they transition to a less intense treatment to prevent the cancer from returning.
If the patient is not eligible for a transplant or has more aggressive cancer, they may undergo the triple treatment for an extended period or take additional anti-cancer drugs like monoclonal antibodies or chemotherapy.
Relapse is a significant concern. Once myeloma returns, previous treatments become less effective at keeping the cancer at bay. For these cases, it may be appropriate to consider a novel immunotherapy called Chimeric Antigen Receptor T Cell Therapy or CAR T therapy.
CAR T therapy is an innovative cell therapy approved to treat myeloma in 2022 and 2024. This breakthrough takes a patient’s white blood T cells, transforms them with gene editing, and reinfuses them into the patient. The edited immune cells have a heightened ability to detect and wipe out cancerous cells and may offer long-lasting protection when other treatments no longer have any impact. According to clinical trial results, 73% to 98% of relapsed myeloma patients respond to CAR T therapy, depending on the product — a beacon of hope for those with few options. Although the FDA is investigating whether CAR T therapies can, in rare instances, cause secondary cancer in patients, the benefits will likely outweigh this potential adverse effect for most people.
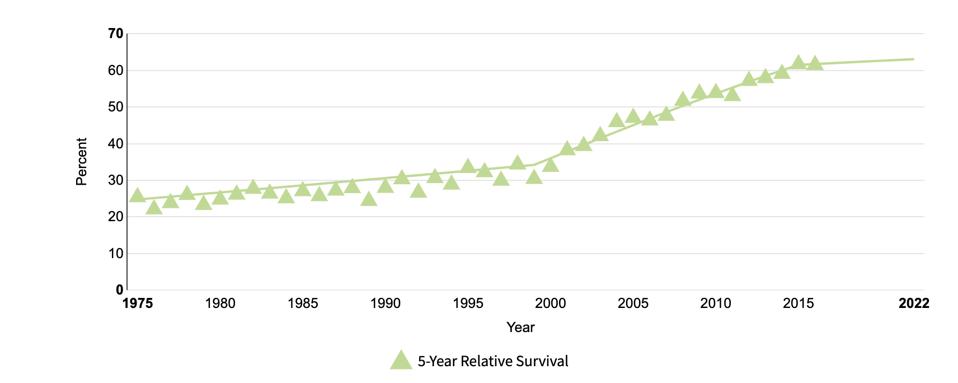
Introducing novel treatments such as proteasome inhibitors, immunomodulating drugs, monoclonal antibodies and CAR T therapy has improved prognoses for myeloma. As shown in Figure 1, the five-year survival rate has increased over the years; today, more myeloma patients than ever are alive five or more years after receiving their diagnosis/starting treatment.
Figure 1: Thanks to improving diagnostics and treatments, five-year survival for myeloma patients has increased over the years (1975-2016).
National Cancer Institute
New Innovations Are On the Way
Multiple myeloma treatments will likely continue to improve, especially in the realm of CAR T therapy. Researchers are investigating ways to improve its efficacy and minimize adverse effects. For example, if CAR T cells target a different protein or target two proteins at once, the treatment may more throughly eliminate cancer cells.
Additionally, several promising clinical trials suggest that CAR T therapy may one day be made with donor cells or with similar mRNA technology featured in the COVID-19 vaccines. Both options, if proven safe and effective, would cut down the most expensive and time-consuming step of the CAR T manufacturing process: gene editing individual batches of blood cells.
Takeaways
Patti Scialfa’s diagnosis has brought new attention to multiple myeloma, a rare and challenging blood cancer. While this disease can significantly affect a patient’s quality of life, the landscape of treatment options is evolving. Breakthrough treatments like CAR T therapy are paving the way for new possibilities, dramatically improving outcomes and offering patients a fighting chance.