An Investigation Into The Basis For The Loss Of Smell As An Early Symptom Of Covid-19
(Posted on Monday, August 3, 2020)
The loss of the sense of smell and taste has proven to be the most reliable indicator of early infection of the SARS-CoV-2 virus. Between 25% and 50% of people report anosmia and ageusia as the very first symptom of Covid-19. Studies of patient records around the world find that the loss of smell or taste is more than twenty times as likely to predict a SARS-CoV-2 positive PCR than a fever, cough, or a stuffy nose. That is very likely because fevers and coughs are associated with many illnesses other than Covid-19.
The loss of smell and taste differs from that associated with most colds. A stuffy nose can, and often does, degrade the sense of smell but not usually that of taste. Moreover, the loss of smell for most colds is not absolute. In the case of most colds, inflamed and swollen tissue blocks odors from reaching the olfactory sensory neurons located high in the nasal cavity, just below the cribriform plate that separates the back of the nasal passage from the brain. In the cases where the virus-induced loss of smell is profound, recovery may take months. The presumed reason is the destruction of the sensory neurons themselves, which regenerate slowly. The acute loss of smell and taste following SARS-CoV-2 infection returns in weeks, not months, suggesting that the underlying pathology may differ.
These observations prompted Harvard scientists to investigate the pathology responsible for the loss of smell following SARS-CoV-2 infection. Their approach was indirect. Rather than tracking infection of the virus itself, they sought to determine what cells in the olfactory tissue harbored two genes used by SARS-CoV-2 to enter cells, the ACE2 surface protein that serves as a receptor, and the cellar protein TMPRSS2 that activates the spike protein of the virus before viral entry.

The results were unexpected. The olfactory neurons that bind and detect the chemicals that produce the sensation of odor express neither ACE2 nor TMPRSS2. Therefore, it is unlikely that the sensory neurons are themselves infected. However, cells that surround and support the olfactory sensory neurons do express both genes and are therefore likely targets of the virus. These are called the sustentacular cells. These cells wrap tightly around the receptor neurons. The authors speculate sustentacular cells are needed to provide an essential function for detecting odor. Virus infection and damage of these cells may account for the transient loss of smell. Presumably, the sustentacular cells regenerate more quickly than the olfactory neurons, accounting for the recovery of the sense of smell within weeks of the viral infection. These studies shed new light on the essential role of the sustentacular cells in odor perception.
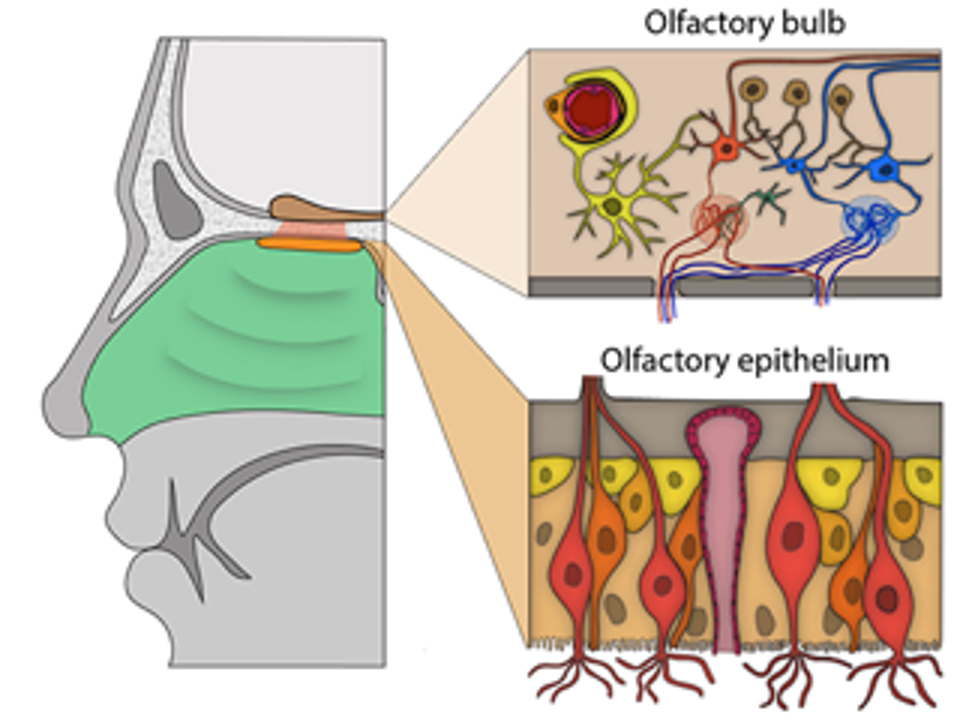
The olfactory bulb and epithelium. Top right: A pericyte (light orange) wraps around a blood vessel (red). Bottom right: Olfactory sensory neurons (light red, orange) surrounded by sustentacular cells (tan) and basal cells (yellow, orange).
HTTPS://HMS.HARVARD.EDU/NEWS/HOW-COVID-19-CAUSES-LOSS-SMELL
The authors also discuss studies that have examined tissues of the human brain for expression of the ACE2 and TRPMSS2 genes. These two proteins are not made by any central system neurons, including those in the olfactory bulbs that receive direct input from the olfactory neurons. They attribute the loss of the sense of smell to damage in the nasal cavity, not the brain. Both ACE2 and TRPMSS2 are expressed on the inner lining of blood vessels that supply the brain, an observation that may account for some of the central nervous system manifestations of Covid-19, including damage to the splenium of the corpus colosseum in adult and children with Multisystem Inflammatory Syndrome-Children (MIS-C).
The conclusions of this report, while compelling, are based on indirect observations. Biopsies of infected tissue that show the virus does indeed infect and replicate in sustentacular cells would be more helpful. An observation of both the damage and recovery of the tissue would be even more compelling.
Also left unexplained is what accounts for the loss of taste. Are the neurons of the taste receptor damaged or, as in the case of the odorant receptors, is the loss of the sense of taste also attributable to damage to the cells that support the taste sensory neurons? There is one cold causing coronavirus, HCoV-NL63, that also uses the ACE2 receptor. Do people who suffer from colds induced by HCov-NL63 also lose the sense of both smell and taste, or one but not the other? This report is sure to encourage further investigation, if not in humans, in sub-human primates.
Originally published on Forbes (July 27, 2020)

