Why We Can’t Rely On Natural Immunity To Protect Us From Covid-19
(Posted on Friday, September 18, 2020)

NEW YORK, NEW YORK – SEPTEMBER 15: People wearing masks carry groceries while crossing the road as the city continues Phase 4 of re-opening following restrictions imposed to slow the spread of coronavirus on September 15, 2020 in New York City. The fourth phase allows outdoor arts and entertainment, sporting events without fans and media production. (Photo by Alexi Rosenfeld/Getty Images)
GETTY IMAGES
There is a question that has crossed all our minds at some point, yet has no satisfactory answer: If I’m infected with SARS-CoV-2, the virus that causes Covid-19, how long am I immune? A more technical way of asking the same question is: How long do anti-SARS-CoV-2 antibodies that bind to the spike protein persist?
While a new study on anti-SARS-CoV-2 antibodies, published yesterday in JAMA, hasn’t much to offer in the way of definitive answers, it does provide some disturbing insight into our natural immunity—or lack thereof—to Covid-19. Compounded with recent reports of reinfection, this study and others like it give us much to think about when it comes to how we move forward in our pandemic response.
When sampling healthcare personnel who work directly with Covid-19 patients at Vanderbilt University Medical Center in Nashville, Tennessee, researchers found that 58 percent of those who tested positive for anti-SARS-CoV-2 antibodies in April tested negative only two months later. Their antibody had levels dropped so precipitously, they were no longer detectable. Even the 42 percent of personnel whose antibody levels remained above threshold still experienced a significant decline (see Figure 1).
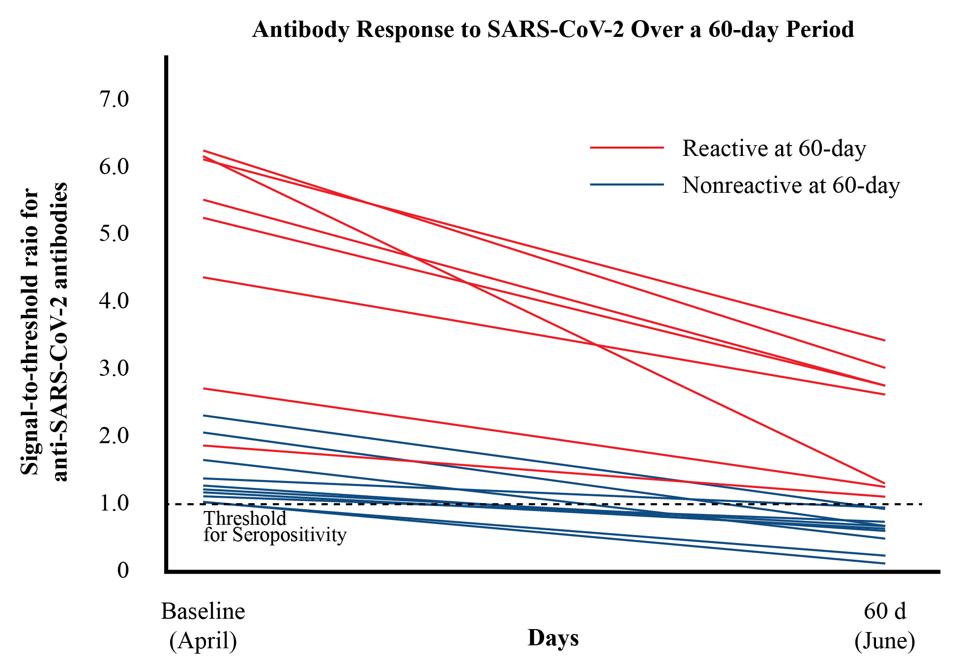
FIGURE 1: A chart tracking decline in antibody levels. Each line represents one patient.
PATEL MM, THORNBURG NJ, STUBBLEFIELD WB, ET AL. CHANGE IN ANTIBODIES TO SARS-COV-2 OVER 60 DAYS AMONG HEALTH CARE PERSONNEL IN NASHVILLE, TENNESSEE. JAMA. PUBLISHED ONLINE SEPTEMBER 17, 2020. DOI:10.1001/JAMA.2020.18796
The targets of the researchers’ assays—in other words, the specific antibodies they were measuring—were anti-SARS-CoV-2 antibodies developed against the viral spike protein. Previous research suggests that these antibodies are critical to the body’s ability to neutralize the virus in patients mildly or seriously ill. Whether their disappearance leaves the body wholly unprotected is far from certain, but it does raise the question of which immune mechanisms do protect us if these antibodies cannot.
We ask this question knowing, thanks to two scientific case studies released last month on Covid-19 patients in Hong Kong and the United States respectively, that it is possible to be reinfected with Covid-19 mere months after having it the first time. While the United States case study, which focuses on a 25-year-old man in Nevada, is still undergoing peer review, it is in our collective interest to take these reports very seriously.
Reinfection is something of a signature move for the coronavirus family, and documentation of this ability dates as far back as the late 1970s and 1980s. If SARS-CoV-2 is both more lethal and more transmissible than its seasonal cold-causing cousins, it would be naive to assume that it wouldn’t be more adept at weaponizing its oldest and dirtiest trick, too. A six-year study of the human coronavirus NL63 (HCoV-NL63), published in 2018, found that people who had contracted the virus in households and hospitals across coastal Kenya were sometimes infected not just once, or twice, but three times.
The authors of the Kenya study speculate that antibodies may have potentiated infection, rather than preventing it, and remark that this was found to occur with SARS-CoV, the virus that caused the first lethal coronavirus pandemic. Such a possibility further complicates our understanding of the role of anti-SARS-CoV-2 antibodies and our immunity to coronaviruses more broadly. Even their tendency to be short-lived isn’t a given. A recent Icelandic study of population antibody levels discovered that about 91 percent of participants who tested positive for Covid-19 retained anti-SARS-CoV-2 antibodies two months after their initial diagnosis.
The reasons why such inconsistencies persist remain elusive, but their implications for how we control and contain Covid-19 are ultimately the same. We cannot rely on natural immunity to protect us from this virus. As long as we don’t have a vaccine, we must use testing, assisted isolation, and other evidence-based public health measures to build up long-lasting and efficacious defenses. Too much is at stake for us to sit back and wait.
(Originally published September 18, 2020 on Forbes)

