SARS-CoV-2 Spike: A Potential Biomarker For Long Covid
(Posted on Friday, June 24, 2022)

Oil painting of a lighthouse leading boats through a storm.
GETTY
Ten to thirty percent of COVID-19 survivors face Long Covid, another battle after initial recovery. PASC, (post-acute sequelae of COVID-19) or PCC (Post-Covid Conditions) encompasses a wide range of symptoms which appear after the acute phase of COVID-19. These symptoms vary widely—from fatigue, chest pain, diarrhea and more—and the mechanisms are not well understood.
At present, there is no clinical test to distinguish Long Covid from several other diseases. And because Long Covid can develop months after mild or asymptomatic COVID-19 cases, even the initial SARS-CoV-2 infection may not be confirmed. This leaves physicians and patients alike at a loss of what to do.
Here inlies the urgent need for a reliable Long Covid biomarker. A biomarker, a measurable indication of a condition or disease, would remove much of the mystery surrounding the complex condition. The ability to confirm a diagnosis would provide well-needed clarity to people who suspect they have Long Covid and to medical professionals trying to provide accurate and helpful patient care. Potential treatment strategies would also be easier to evaluate if the mechanism was more understood.
A New Biomarker Study
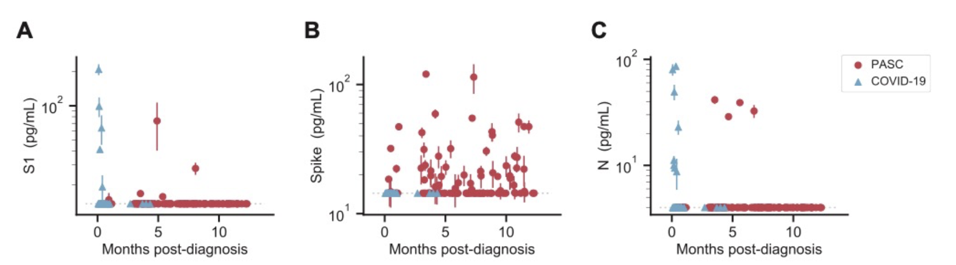
Swank et al. discuss a potential biomarker for identifying Long Covid in their preprint, Persistent circulating SARS-CoV-2 spike is associated with post-acute COVID-19 sequelae. The researchers collected blood samples from confirmed COVID-19 patients—37 with a PASC diagnosis, 26 without. They analyzed the plasma for concentrations of SARS-CoV-2 antigens using an ultra-sensitive single molecule assay (SIMOA) pioneered at the Walt lab. The SIMOA technique allowed the team to detect full length spike (S), S1 subunit of spike and nucleocapsid (N) at around 1000x higher sensitivity than typical ELISA assays.
Figure 1. SARS-CoV-2 antigen levels versus time. The concentration of S1 (A), spike (B), and N (C) measured in the plasma of individuals over time after diagnosis with PASC or COVID-19 following SARS-CoV-2 infection. Multiple data points may correspo
SWANK ET AL.
Of the three antigens, the study’s findings attribute the full SARS-CoV-2 spike antigen as the best biomarker candidate. The full length spike (S protein) was detected in 60% of PASC patients, with many displaying sustained spike levels over a period of several months. The full length spike was not detected in COVID-19 only patients during the acute phase of infection. The results highlight the S protein’s potential as a biomarker of Long Covid. These findings, if reproduced in a larger study, could significantly improve the study and treatment of Long Covid.
Long Covid and Possible Viral Reservoirs
Intriguingly, Swank et al. detected free floating S1 in only 20% of their Long Covid cohort. It’s unusual to see full length spike circulating the serum in such an absence of S1. The S protein is composed of two subunits: S2, which is anchored in the SARS-CoV-2 transmembrane; and S1, which sits on top and contains the receptor binding domain. For most strains of SARS-CoV-2, the complete spike precursor protein is cleaved upon viral exit, freeing S1 to float and leaving the S2 attached to the transmembrane.
Why, then, was full S protein detected more than S1? A possible explanation has been observed by researchers who found that uncleaved, full length spike protein circulates while attached to exosomes. Maybe these small extracellular membrane vesicles, equipped with the entire S protein, are present in Long Covid patients.
Swank et al.’s observations raise another puzzling question: why is the S protein still circulating despite its short half-life in the blood? It seems the spike protein is being made, although how is uncertain. One hypothesis argues for the existence of a persistent reservoir of active virus. This reservoir could be replicating SARS-CoV-2 virus at low levels. An earlier study found a reservoir in the gastrointestinal tract of children who developed post-Covid related MIS-C, but post-mortem tissue analyses revealed SARS-CoV-2 RNA and protein expression in several other tissues, suggesting reservoirs may also be found elsewhere in the body. Another possibility is that subgenomic RNA capable of producing spike protein persists in the absence of full viral replication. In this regard, it’s worth noting some coronaviruses produce defective interfering viruses which account for persistence of subgenomic RNA fragments in infected subcultures.
Other Markers of Inflammation
A previous study also used SIMOA technology to search for potential biomarkers of COVID-19 related damage. In this study from the NYU Grossman School of Medicine, Frontera et al. found that individuals hospitalized for COVID-19 displayed elevated levels of inflammatory neurodegenerative biomarkers in their blood—total tau, Neuro-filament light, Glial fibrillary acidic protein and others. Those hospitalized with new neurological symptoms displayed higher Ubiquitin carboxy-terminal hydrolase L1 and ptau-181. These markers are also characteristic of late-stage Alzheimer’s disease.
Both studies observed typical cytokine IL-6 levels in their populations, suggesting it may be best to prioritize other inflammatory biomarkers.
It would be interesting to test for these neurodegenerative markers in Swank et al.’s Long Covid patients. The Long Covid cohort was much younger (median age of 46 compared to 71) and was not specifically selected for neurological symptoms. Another difference is severity: only 21 of the 63 total participants were hospitalized for COVID-19. Considering brain fog and memory loss are common complaints for Long Covid, these biomarkers may warrant additional investigation.
A Hopeful Beginning
Swank et al. bring promise to Long Covid biomarker research. Although the cohort was small, the study provides strong support for full spike as a Long Covid-specific indicator. If clinically adapted, physicians would finally have a conclusive means to diagnose the condition; people with Long Covid would no longer be told their symptoms originate from psychosomatic disease; and effective treatments could be tailored to target the possible viral reservoirs in Long Covid patients. Additional studies are needed to validate these preliminary Long Covid associated biomarkers. Future efforts should follow large patient populations for a long time. The SIMOA methods may offer a convenient tool for such studies.