Gene Therapy Solutions For Age-Related Macular Degeneration
(Posted on Sunday, August 6, 2023)
Originally published on Forbes on 8/1/2023
This story is part of a series on the current progression in Regenerative Medicine. This piece is part of a series dedicated to the eye, and it marks the third of a three-part series on dry age-related macular degeneration. Other pieces in the series include protein therapies, stem cell therapies, and omega-3 for macular degeneration.
In 1999, I defined regenerative medicine as the collection of interventions that restore to normal function tissues and organs that have been damaged by disease, injured by trauma, or worn by time. I include a full spectrum of chemical, gene, and protein-based medicines, cell-based therapies, and biomechanical interventions that achieve that goal.
Age-related macular degeneration affects millions worldwide and features wet and dry subtypes. Although some patients’ visual acuity may remain the same, disease progression often leads to vision loss. In fact, the dry form often leads to geographic atrophy, an irreversible condition resulting in vision loss.
The search for effective treatments has been ongoing, and a team of international researchers published a comprehensive review in Clinical Ophthalmology to explore the latest investigational therapeutics for this debilitating disease. Gene therapy is currently one of the trailblazing treatments for dry age-related macular degeneration under research.
Dry Macular Degeneration Leads to Geographic Atrophy
Dry age-related macular degeneration is a progressive retinal disease that results from damage to the macula, the part of the eye responsible for central vision and the ability to see fine details.

The disease progresses slowly over time. It also has three stages: early, intermediate, and late.
Late-stage dry macular degeneration can lead to the onset of geographic atrophy. Geographic atrophy causes retinal cells to waste away and die, creating patchy areas in the retina that cause blind spots in vision. These areas of dead and dying cells appear in retinal images and resemble a map, which is why it’s called geographic atrophy. It can impact one or both eyes. It is estimated to impact around 1% of the population in the United States and over 8 million people globally.
Although the exact cause of geographic atrophy is unclear, it likely results from genetic and environmental factors. Risk factors associated with age-related macular degeneration and geographic atrophy include smoking, age, and family history. Fortunately, there is now an FDA-approved treatment for geographic atrophy.
An Approved Geographic Atrophy Treatment
In 2023, the FDA approved pegcetacoplan or Syfovre® for treating dry age-related macular degeneration. This medication works by inhibiting a protein found in the complement system. The complement system is part of the immune system and is responsible for attacking foreign bodies. It recognizes, tags, and eliminates any foreign particles. In dry macular degeneration, an overactive complement system damages retinal cells leading to blind spots in vision.
Syfovre® prevents the complement system’s C3 protein from becoming out of control. Properly managing this slows down retinal damage, halting the progression of geographic atrophy.
Clinical trials of Syfovre® showed that injections can slow the growth of sores, thus preserving vision. The medication is injected directly into the clear gel-like substance that fills the eye. As with any injection, the risk of inflammation and infection is increased. Apellis has reported an increased incidence of eye inflammation during clinical trials, which led some experts to question the risk-to-benefit profile of the drug.
One such expert, Demetrios Vavvas, an ophthalmology professor at Harvard Medical School and the director of the Retina Service at Massachusetts Eye and Ear, expressed his concern in an interview where he said, “As the potential benefit goes up, the risks go up, and the benefits are potential. The risks are real”.
Vavvas’ concerns were validated on July 29, 2023, as Apellis’ lead researchers presented the safety and efficacy of Syfovre® at the American Society of Retinal Specialists Annual Conference. The presentation led to the safety committee advising the American Society of Retinal Specialists to publish a letter of concern regarding increased cases of ocular inflammation. More specifically, six instances of occlusive retinal vasculitis were reported.
Retinal vasculitis is a potentially blinding inflammation of the eye, and at least one of the six impacted individuals reported significant vision loss after receiving their injection. Apellis said that the incidence of this particular eye inflammation aligns with their findings in clinical trials with an estimated rate of 0.01% per injection.
Still, there is cause for concern considering individuals must receive these injections every 25 to 60 days, depending on severity, for this treatment to be effective. The inflammation and retinal vasculitis cases have not been tied to any particular batch of medication or manufacturing issues. However, patients reported the effects two weeks after their first Syfovre® injection.
Apellis is currently investigating these reports concerning their geographic atrophy medication, but what if we could treat dry age-related macular degeneration before it becomes geographic atrophy?
Current Options for Those with Dry Macular Degeneration
Age-related macular degeneration currently lacks a definitive cure, but various treatment options are available. Among these, nutritional supplements stand out.
Two studies conducted by the National Eye Institute, a branch of the National Institute of Health, explore the relationship between vitamins and eye health. More specifically, these studies, known as Age-Related Eye Disease Studies, or AREDS and AREDS2, determined whether vitamins and minerals could slow the progression of age-related eye diseases like dry macular degeneration.
The initial AREDS study indicated that vitamins C and E, copper, and zinc successfully slowed the progression of macular degeneration. AREDS2 expanded this by including lutein, zeaxanthin, and omega-3 fatty acids, ultimately showing an even more pronounced effect in slowing down the disease. Although nutritional supplements cannot cure macular degeneration, they are a viable option to slow its progression. Acknowledging that dietary supplements do not effectively manage late-stage dry macular degeneration or geographic atrophy is also essential. This is why gene therapies are being investigated as potential treatments for the disease.
Gene Therapy For Dry Age-Related Macular Degeneration
Scientists are currently studying the effectiveness of gene therapies in preventing or treating dry macular degeneration. Cutting-edge gene therapies, GT-005 and HMR59, are developing as promising treatments.
GT-005 is an investigational gene therapy developed by Gyroscope Therapeutics. This therapy aims to slow the progression of geographic atrophy caused by dry age-related macular degeneration by increasing complement factor I levels in the retina. CFI is a protein that regulates inflammation. Recall the discussion of Syfovre from earlier. Some parts of the complement system can become overactive, leading to macular degeneration and geographic atrophy. Other parts, like CFI, can be underactive and lead to the same problem. Maintaining a balance of complement is essential for preventing age-related macular degeneration.
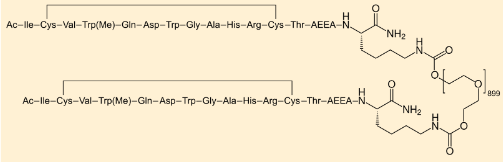
GT-005 employs an adeno-associated viral vector (AAV) to enhance CFI expression levels. An AAV is a small virus modified to deliver therapeutic genes to cells; in the case of GT-005, the AAV deposits therapeutic genes in the cells of the retina. This design allows the therapy to be a one-time treatment delivered under the retina. GT-005 is currently undergoing evaluation in Phase I and II trials.
The other primary gene therapy currently being investigated for treating dry age-related macular degeneration is HMR59 by Hemera Biosciences. HMR59 focuses on preserving vision in those with late-stage geographic atrophy. Its purpose is to enhance the capacity of retina cells to produce a soluble version of CD59 protein.
CD59 is one of the proteins that protect the retina from damage from the complement system. As we know, any imbalance in the complement system can lead to the death of light-sensitive cells in the back of our eyes and vision loss. By increasing the activity of CD59 using gene therapy, HMR59 can protect these vital cells from destruction due to complement-induced damage.
Like GT-005, HMR59 is a one-time treatment. Researchers administer the medication by injecting it into the transparent gel-like substance inside the eye. At the time of writing, HMR59 phase I studies are complete, and phase II has begun. There is also another phase I trial starting to see if there are any beneficial effects of HMR59 on wet age-related macular degeneration.
Early results from clinical trials are promising, especially concerning the sustained expression of therapeutic proteins. Thorough research is required before these therapies can be released to avoid unintended effects. Gene therapies represent a revolutionary shift in treating age-related macular degeneration, geographic atrophy, and other age-related eye diseases.
To learn more about the eye, read more stories at www.williamhaseltine.com

